Schistosomiasis is a parasitic disease caused by blood flukes. There are two forms of the disease, intestinal schistosomiasis and urinary schistosomiasis, Schistosoma haematobium being the species of fluke that is responsible for the latter.
Urinary Schistosomiasis
Infection occurs when people use water sources contaminated with larval forms of S. haematobium that have been shed from their snail intermediate hosts.
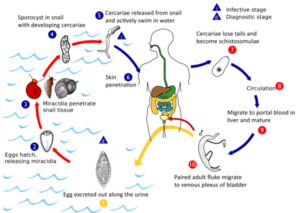
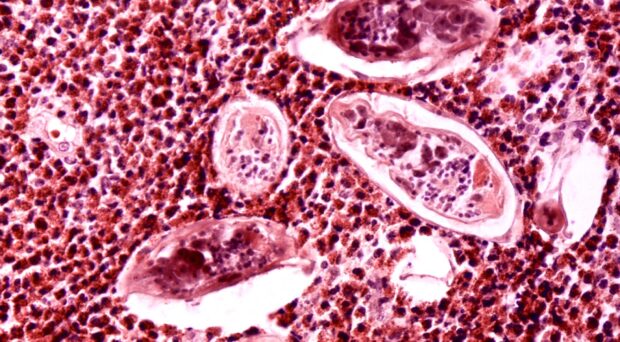
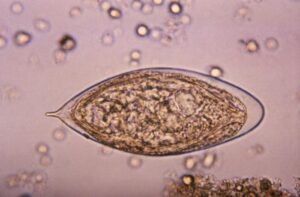
Larvae burrow through the skin, transform into adult worms and take up residence in the blood vessels surrounding the bladder. Some of the eggs released by female worms pass out of the body in the urine, hatch on contact with fresh water and continue the parasite’s life cycle if contact with a specific species of snail is made. However, many of the eggs are retained in the body tissues, causing immune reactions and organ damage.
Blood in the urine is the classical symptom of urinary schistosomiasis. In long-term infections, the deposition of eggs can lead to fibrosis of the bladder or urethra, and kidney damage. This pathology can progress to cancer of the bladder or kidney. In females, eggs can migrate to the genital tract, causing female genital schistosomiasis (FGS).
Female genital schistosomiasis
The inflammatory response to fluke eggs changes the genital tract mucosal tissue due to the formation of granulomas and abnormal development of blood vessels.
This, in turn, causes irritation, discharge and vaginal bleeding. Clinical manifestations can include infertility, ectopic pregnancies and abortions, and lead to an increased risk of the acquisition of HIV infection. Girls can be infected from an early age and repeated contact with contaminated water results in recurrent infections and a build-up of egg deposition. Between 30% and 75% of females with urinary schistosomiases are estimated to also develop FGS.
A recent review in the British Medical Bulletin estimates this neglected disease affects 30-56 million females, mostly in sub-Saharan Africa. The authors note the lack of surveillance for FGS within normal schistosomiasis control programmes. They point out the need to integrate standardised screening and diagnosis within sexual reproductive health programmes, together with an economic assessment of new, community-based diagnostic strategies.
A neglected public health problem in Tanzania
Tanzania ranks second only to Nigeria for the prevalence of schistosomiasis in Africa, with the urinary form accounting for two-thirds of the cases. However, there is a dearth of data regarding FGS that might inform control programme managers and policy makers. This concern prompted the conduction of a scoping review of published studies by Gladys Mbwanji and colleagues. They focussed on the epidemiology of FGS in Tanzania’s mainland and Zanzibar islands, where urinary schistosomiasis is prevalent in girls and women living in marginalised rural communities. Their study posed questions from a public health viewpoint and looked for gaps in knowledge.
Peer-reviewed papers, published between 1981 and 2022, were considered, and a quality assessment of them was carried out using a risk of bias tool. This reduced the number of papers to be considered to 20. They grouped these papers into community-based studies, hospital-based studies, case studies, diagnostic studies, and qualitative studies.
Community-based studies had been conducted in northern Tanzania in 1998 and 2000. In the first study, 40% of 543 women had urinary schistosomiasis, 62% of them also had FGS, while 23% had eggs in the cervical tissue, but not in their urine. In 2000, the overall prevalence of urinary schistosomiasis amongst 657 women was 36%, and the incidence of FGS had declined to 37%, with three quarters of them exhibiting cervical lesions. In north-western Tanzania, studies linked common symptoms of FGS with sexually transmitted infections and considered the effect of mass treatment with praziquantel.
Hospital-based studies of tissues collected during biopsies or surgery associated abnormalities in the genital tract with the presence of schistosome eggs, but a link between FGS and cervical cancer could not be proven because of the presence of human papillomaviruses in all cases.
The one published case study reported that a single dose of praziquantel cured the symptoms of a girl with eggs in her urine and embedded in her labia.
The results of several studies of FGS diagnostic tests were discussed, including cytological and biopsy examination, with the recommendation not to use cervical biopsy if there was a danger of HIV infection while the cervix healed. A positive result for a simple urine reagent-strip test to detect haematuria was found to identify 65% of females with eggs in their urine but must avoid blood contamination during menses. Positive screening of vaginal lavage fluid for Schistosoma DNA corresponded with its presence in urine, but not with the detection of eggs there, or in genital tract tissue.
Lastly, although there was a relatively good understanding of urinary schistosomiasis in communities, knowledge of FGS was severely lacking. The authors identified a need for community education and in-service training for health workers, particularly in the islands of Unguja (Zanzibar) and Pemba.
Conclusions
The authors observed that FGS is common in heterogeneously dispersed areas of northern and north-western Tanzania that exhibited different S. haematobium transmission intensities. Up-to-date epidemiological studies were very limited, and there were none for many parts of the country. More studies are urgently needed to better inform interventions.
They recommend that mass administration of single dose praziquantel to school children needs to be extended to adolescent girls and women, and a greater understanding of the impact of this treatment on FGS is required. Finally, the diagnosis and treatment of FGS needs to be integrated into primary health care services.
Clearly FGS is a neglected tropical disease in need of further attention.

Comments