India is historically a malaria endemic country. It holds the distinction of being the site of the discovery by Noble Prize winner Sir Ronal Ross that established the malaria parasite cycle through Anopheles mosquitoes as the definitive host, and the spectacular success of malaria control during 1960s. India is a vast country and disease epidemiology is complex, with various paradigms of transmission, multiplicity of vectors, varied terrain and contextual determinants.
Malaria Elimination in South-East Asia
Malaria elimination is a buzz word and, given the present-day intervention tools, it has become reality. The world malarial map is shrinking with many countries having acquired malaria-free status. Among these, in the South-East Asia Region (SEAR) of the World Health Organization (WHO), the Maldives (2015) and Sri Lanka (2016) have been certified to be malaria free and Bhutan is fast approaching towards elimination in the foreseeable future.
India too is marching ahead with a goal of malaria elimination by 2027 (three years ahead of the global agenda).
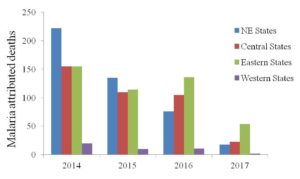
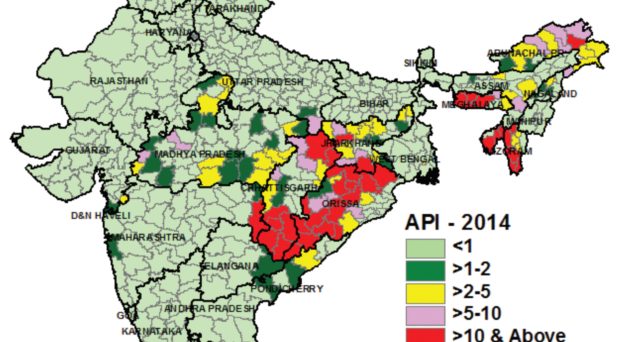
Impressive gains have been reported in reducing morbidity; largely attributed to a sharp decline in cases (80% drop in 2018 compared to 2017) in the state of Odisha (formerly Orissa) contributing 40% of the cases in the country. Nevertheless, in SEAR member countries, India still contributes most cases (80%) with nearly a billion population at risk.
Potential for elimination in India
India holds the capacity for elimination due to its massive expansion of health infrastructure, strengthened by the Integrated Disease Surveillance Project (IDSP), the National Health Mission (NHM), skilled workforce and rejuvenated political commitment to beat the daredevil. In this context, the induction of Accredited Social Health Activists (ASHA) workers have brought a sea change in disease surveillance, ensuring case detection and treatment right at the door step, well in time and place, building confidence in the endemic communities.
India has already drawn a strategic plan of action for malaria elimination at the district level for task to be completed in a phased manner, including preventing re-establishment of local transmission and maintaining malaria-free status by 2030 and beyond.
However, the road ahead to elimination is fraught with many bottlenecks. So much so that WHO has listed India among 11 ‘high burden to high impact’ countries for contributing 4% of the global malaria burden.
Challenges ahead
Malaria elimination in India is a herculean task and has regional implications.
Amidst a myriad of challenges common to many countries, development and spread of multiple insecticide resistance in disease vectors and emergence of drug-resistant malaria stands out to be the foremost. To address these issues, vector surveillance (anti-vector) along with monitoring therapeutic efficacy of antimalarials (anti-parasite) measures should be the continuing activities to mitigate disease onslaught – an activity that would be of paramount importance post-elimination.
The upgrading of treatment policy based on artemisinin-based combination therapy (ACT) in space and time have had a tangible impact on disease transmission-reduction in high-risk pockets that were formerly intractable.
Furthermore, the advent of long-lasting insecticidal nets (LLINs) have proven a boon to the control programme producing overwhelming community acceptance and operationally feasible technology in hard-to-reach endemic communities. These nets have been assessed to be durable and retain residual bio-efficacy for net serviceable life of just about 3 years; beyond which there is a need to make adequate provision for replacement of torn nets for uninterrupted protection. Nevertheless, population coverage remains miniscule compared to what is needed for protection of communities at any risk. Innovative technologies that are environmental-friendly, community-based and sustainable are, however, mandated to overcome insecticide resistance and mitigate outdoor transmission
Equally important would be to enhance disease surveillance to include detection and treatment of asymptomatic/sub-patent parasitaemia to disrupt transmission.

There is a hidden sea of asymptomatic malaria entrenched in high-risk marginalized communities spread throughout India, yet unattended, as there are no standard guidelines for diagnostic procedures and treatment aspects aimed at carriers.
India shares long international border with many countries of which Bhutan, Nepal, Myanmar and Bangladesh are of immediate significance. This calls for concerted action to thwart entry of drug-resistant strains or, more so, to prevent re-establishment of transmission in malaria-free territories. These borders are porous and prone to fulminating disease outbreaks owing to mixing of strains and consequent heightened morbidity. The border with Myanmar in northeast India, in particular, is seen as corridor for spread of drug-resistant varieties emanating from Cambodia, and onward transmission to peninsular India and westwards.
Reasons for hope
Taking cognizance of the issues related to cross-border malaria, India is a member, with the Asia Pacific Malaria Elimination Network (APMEN) of countries and signatories to the Asia Pacific Leaders Malaria Alliance (APLMA) for shared experiences and coordinated action towards common goal of defeating malaria.
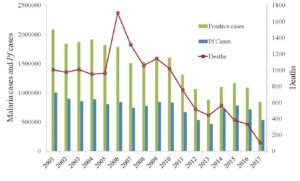
Given the steady declining transmission of malaria in India for the past few years there is renewed optimism achieving ambitious goal of malaria elimination in due time. What is needed is the political commitment for sustained allocation of resources ensuring universal coverage of interventions, human resource development in keeping abreast with the latest developments, monitoring and evaluation for informed decisions, inter-sectoral convergence and above all empowering communities, making it a community-driven enterprise.
India has conquered polio against all odds and can beat malaria as well. Eliminating malaria in India (the second largest populous country of the world) would be a great leap forward and the highest achievement of the century in public health.

Comments