Female genital schistosomiasis (FGS) is a disabling and neglected gynaecological disease caused by the egg-deposition of the Schistosoma haematobium parasite in the genital tract. Transmission is facilitated by freshwater snails, as an intermediate host, and it occurs when a person is in contact with contaminated fresh water. FGS is a remarkable inflammatory disease. Entrapped eggs in the genital tract, result in a recruitment of inflammatory cells and cytokines with a granulomatous reaction, as the body tries to contain the progression of the infection. The clinical consequences are a direct result of that inflammatory process and manifest with vaginal discharge, lower abdominal pain, pain and discomfort during sex and bleeding in between menstrual periods. Untreated infection may lead to infertility, genital ulcers, miscarriage, ectopic pregnancy, post-coital bleeding and an increased risk of acquiring HIV and possibly cervical cancer. Research is lagging behind, and there is an urgent need to increase knowledge and options to diagnose this disabling disease.
In my own practice as a specialist Gynaecologist, working at Queen Elizabeth central hospital in the city of Blantyre in Malawi, I have seen women who have been referred from primary and secondary health facilities with complaints of abnormal vaginal discharge. These women usually have had multiple injections of antibiotics but without much improvement. Sometimes they are referred because they have lesions suspicious of cancer in the genital tract. On multiple occasions we have sent tissue samples from the genital tract to either confirm a clinical diagnosis of cervical cancer or some other disease. Interestingly, some of the biopsy results have shown Schistosoma eggs with or without cancer findings, but even in the presence of FGS, the clinical importance is placed heavily on the alternative diagnosis, minimizing the contribution of this parasitic disease on sexual and reproductive health.
In this post, I will be sharing my personal experience working on an FGS project, the MORBID-FGS study, a multi-partner collaboration between, Centre for Health, Agriculture, Development Research Consulting (CHAD) in Malawi, the London School of Hygiene & Tropical Medicine and the Schistosomiasis Control Initiative Foundation (SCIF) in the UK. The study’s main objective was to quantify the burden of disease of FGS in two areas in Malawi, one with high prevalence of schistosomiasis (Nsanje) and one with low prevalence (Chikwawa). The study included women of reproductive age from age 15 to 59, sexually active and nonpregnant. In November 2020 we started recruiting women from an ongoing larger study (MORBID) aiming to find associations between different levels of schistosomiasis endemicity and clinical morbidity. Eligible women were given a questionnaire and were asked about symptoms pertaining to their reproductive tract and invited to come for a clinical review. At the clinic, nurses performed a genital examination of the women, examining the vulva, vagina and cervix, first with the naked eye and then with a hand-held colposcope to magnify any abnormalities. Swabs and lavage samples were obtained from the lower genital tract and processed for Schistosoma DNA detection.
During the first few weeks into recruitment, in Nsanje district, an area with high prevalence of schistosomiasis, our team met a young girl, aged 15 who lived in a part of Nsanje called Fatima. The main source of water for daily activities for her community is the Shire river. It is also a hub for agricultural activities such as farming and fishing. Access to clean portable water and sanitation is limited. The fresh water is a good habitat for the snails that act as the intermediate host for schistosomes.

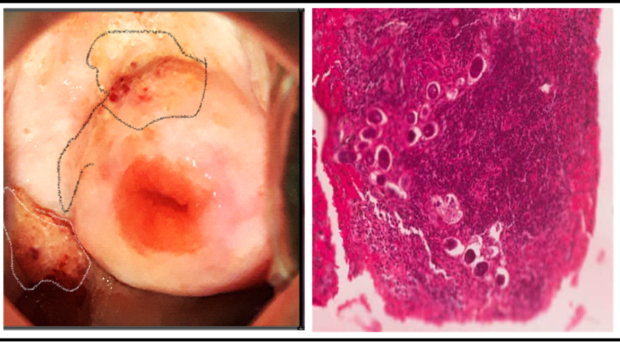
Just like other girls, she had been invited to participate in the MORBID FGS study. She was about to start secondary school and her growth was what was expected at this age. She had an otherwise non-remarkable gynaecological or history. Upon undergoing visual screening with a colposcope for female genital schistosomiasis, a suspicious mass with contact bleeding was discovered on her vaginal wall. Exercising caution, I took a biopsy to rule out a possible choriocarcinoma (a malignant tumor of the uterus). The histopathological results of the biopsy revealed that the mass was a collection of S. haematobium eggs. She was treated with praziquantel, the only available drug to treat all types of schistosomiasis. If this girl hadn’t been part of this study, she would have likely been treated for sexually transmitted infections since the symptoms are indistinguishable, and her FGS would have remained untreated with potential dire impact to her sexual and reproductive life.

The images obtained by colposcopy allowed us to see the effects of schistosomiasis only in the lower genital tract as it is unable to image deeper genital organs like the uterus, fallopian tubes or ovaries. Therefore, it is difficult to quantify the extent of the clinical disease just by imaging the cervix and vagina. In addition to the clinical diagnostic limitations, many women go undiagnosed due to a lack of awareness of FGS by health care workers. Another limiting factor is the lack of access safe water and sanitation.
Women also don’t get appropriately treated due to the absence of praziquantel in most health facilities in Malawi and elsewhere. PZQ is seen as a ‘control’ drug and only gets used occasionally in the health system to treat urinary or stool confirmed schistosomiasis.
As long as these issues are not adequately addressed, schistosomes will remain a threat to women’s sexual and reproductive health. I have now learned to identify FGS and I have also realized that many of my colleagues continue to practice without thinking about it. I would like to increase awareness in the medical education in Malawi by teaching nurses, doctors and gynecologists about my experience. I continue to be part of the FGS research efforts in Africa as an expert reviewer in both Malawi and Zambia.

Comments