Frailty

Dr. Emma Grace Lewis presented an interesting study from a Tanzanian cohort, and found a positive association between age and the Frailty Index. Frailty was also more prevalent in women, yet the women in this region live longer than the men – highlighting the so-called male-female health survival paradox.
Dr. Ying Lim at Duke-NUS presented an interesting study on the application of a simple frailty index (FRAIL) in a community setting and compared the results to those obtained using the ‘gold standard’ scales: the Fried phenotype and the Frailty Index. FRAIL had low sensitivity but high specificity; it was good at picking up robust frailty, but less so for pre-frail and frail individuals.
Prof. John Gladman presented an interesting discussion on what could be considered an appropriate term for a state that is the opposite of frailty, deeming ‘resilience’ to be an apt choice. He also expounded on the importance of starting prevention from a young age, as frailty is a lifecourse issue.
What about interventions to tackle frailty? With respect to whether or not nutrition-based interventions are effective, Prof. Sian Robinson discussed the evidence which favors nutrient combinations over single supplements, and highlighted that there is currently a lack of evidence regarding the impact of these interventions on physical function.
Likewise, the evidence for dual supplementation and exercise training interventions is inconsistent. Looking at the components of physical function, Dr. Carolyn Greig presented the evidence supporting the benefits of exercise for increasing muscle mass, strength and physical performance (though studies are limited and, again, the evidence is mixed). Prof. Miles Witham also noted that, in this regard, most evidence is for resistance (over endurance) exercise.
Looking at social and environmental factors is important, too. Prof. Martin Vernon noted that frail people are more likely to live in deprived areas, and the prevalence of frailty overlaps with socioeconomic factors like poor housing and fast-food outlet maps.
Acute sarcopenia
To date, ‘acute sarcopenia’ hasn’t been fully characterized, but it is known that a heightened inflammatory response exasperates the condition. Dr. Carly Welch presented results from a pilot study, in which inflammatory markers – most notably DHEA-5 and hsCRP – were measured in older patients undergoing elective colorectal surgery. The results showed less decline in gait speed in those with higher baseline DHEA-5, and likewise less reduction in BATT (bilateral anterior thigh thickness) in those with higher baseline hsCRP.
Palliative care
As shown by Dr. Caroline Nicholson, the palliative care needs of frailty patients (when compared to the standard population) reflect not so much a different set of needs but rather a different pace of change (and thus a different pattern of care), and possibly a different set of priorities clustered around functionality and keeping on ones feet; thus, we need to adapt to this to provide quality end of life care.
Dr. Maggie Keeble gave a nice talk on the need to recognize triggers that would prompt the discussion of end of life care. Compared to other chronic conditions (such as cancer), the triggers for this discussion in frail patients are not as obvious so we need to be better at picking these up; these include a diagnosis of moderate/severe frailty. The language used for this discussion is key, such as saying the patient is approaching the end of their life (appropriate given that the timescale can be long and the cause may be reversible). She also encouraged people to add frailty to the death certificate as the primary/secondary cause of death so it is considered a legitimate cause.
Falls assessments
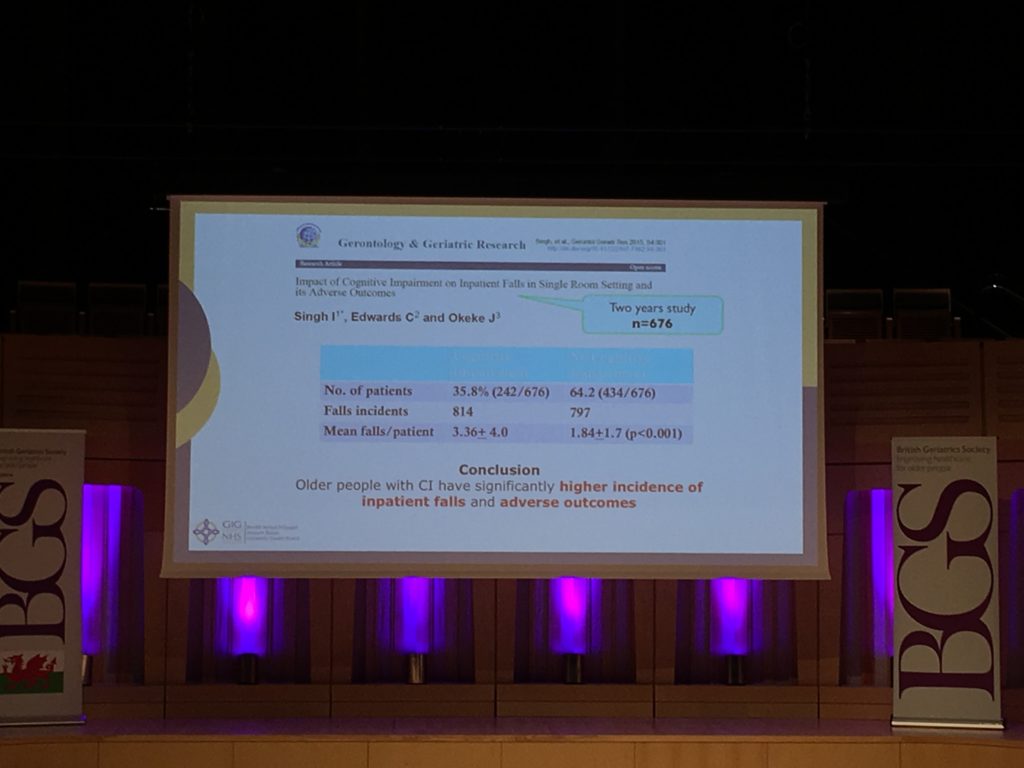
Both Dr. Julie Whitney and Dr. Inderpal Singh presented data on geriatric inpatient falls. Dr. Whitney discussed the severe harm caused to older patients who suffer falls, such as an increase in distress and a decrease in confidence; thus, it is important to identify those at high risk of falls and prevent this, and so the National Audit of Inpatient Falls (NAIF) was set up to monitor prevention care in acute hospitals. As of last year, its remit now extends beyond this setting, and will be focusing on patients who’ve sustained a hip fracture through a continuous audit (as opposed to the previous ‘snapshot’ approach).
Dr. Singh noted that the prevalence and harm of inpatient falls is 3-times higher in those above 65 years of age, and older individuals with a cognitive impairment also have a greater incidence of falls and adverse outcomes. A further issue he highlighted is that inpatient falls were considered a ‘nursing problem’, as opposed to a ‘medical problem’, meaning that discussions on the topic are often siloed. Thus, effective interventions, quality initiatives and collaborative efforts are needed to overcome these problems.
Emerging themes from this meeting include the need for more (and better quality) studies with respect to interventions for frailty, the importance of using appropriate language when discussing frailty and palliative care, and the need for effective quality initiatives and falls prevention strategies.
Comments