
Endemic zoonotic infections, which jump between animals and humans and are present at a stable level of infection in the population, pose a substantial, sustained public health and economic burden. They often disproportionately impact marginalised communities in low-income countries; therefore, it is essential that these endemic zoonotic infections are not forgotten. One such zoonotic infection, widely endemic across Central, South America, sub-Saharan Africa and Asia is the pork tapeworm Taenia solium.
The life cycle of T. solium is complex. It passes through pigs as a larval-stage infection and into humans, where the large adult tapeworm develops and lives in the human intestine. Humans may also develop the larval-stage infection, whereby cysts primarily reside in the central nervous system and can lead to chronic infection and morbidity, a condition called neurocysticercosis (NCC). Several studies have implicated NCC as the leading preventable cause of epilepsy in low- and middle- income countries, accounting for approximately one third of epilepsy cases in countries where T. solium is endemic.
T. solium is a complex One Health problem that thrives on the close interaction between pigs, people, and places.
One Health has been defined as:
“The recognition that the health of humans, animals and ecosystems are interconnected”.
T. solium provides a clear example of how these three elements—humans, animals and ecosystems—are so closely connected (see figure). A typical endemic area includes free-roaming pigs in rural farming communities, which exposes the pigs to the infective stages of T.solium in the environment. In many communities where the disease is endemic, humans often practice open defecation, which subsequently results in the release of the infective stages into the wider environment. Poor sanitation also leads to humans ingesting T. solium eggs and this ultimately leads to NCC infection. Ineffective meat preparation and minimal meat inspection of carcasses drive human exposure to T. solium larvae within infected pork meat. So, while the disease system is clearly complex, the involvement of humans, animals and the environment in transmission processes also provide a range of different options for control.
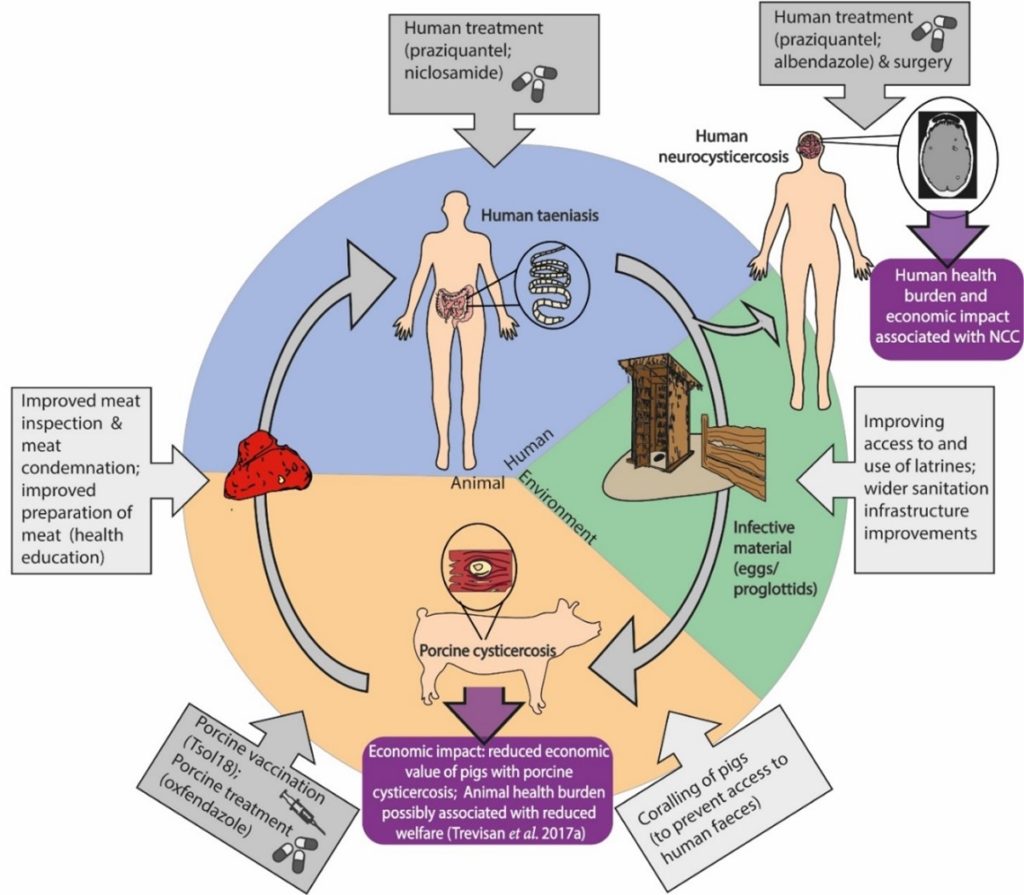
Effective solutions, especially over the shorter-term, will require a cross-sectoral approach involving interventions in pigs, humans and the environment.
The new World Health Organisation (WHO) neglected tropical disease (NTD) 2021-2030 roadmap sets key milestones for T. solium based on measuring the number of countries achieving “intensified control” in hyperendemic areas by 2030. The tools currently available for control include treatment of humans, treatment of pigs and vaccination of pigs. All of these tools have shown efficacy in the field. For example, a large pilot study in Madagascar demonstrated the ability of a three-year human mass treatment strategy using the drug praziquantel, to dramatically reduce the level of adult tapeworms that live in the human intestine. These results are encouraging, however it is important to note that infection quickly rebounded after the treatment ceased. Combined treatment and vaccination of pigs in Tanzania has also shown success in substantially reducing cysticercosis infection in pigs. While interventions in pigs or humans separately are efficacious, attaining more ambitious control or elimination targets will likely take a combination of these intervention in both hosts and the environment.
A more intensive intervention programme which can attain the NTD roadmap T. solium milestones over the short-term might be a more attractive option to policymakers. Achieving these control efforts over a few years, or shifting ambitions towards elimination rather than control (with elimination of transmission proven possible in northern Peru) will likely require a One Health approach, targeting chemotherapeutic interventions in both the pig and human hosts. Once elimination is achieved in specific geographic areas, further challenges may arise around re-importation risk of T.solium infection through movement of pigs and humans.
Delivering a One Health strategy for T.solium does not necessarily restrict an approach to pharmaceutical interventions. Leveraging and combining efforts with on-going water, sanitation, and hygiene (WASH) activities, which are focussed on providing access to clean water and encouraging use of latrines, will also provide a benefit to T. solium control. One Health principles also extend to finding sustainable, innovative financing mechanisms to support control programmes.
Existing large-scale NTD programmes may also impact T. solium infection in co-endemic areas, such as human mass treatment programmes which also use praziquantel to control schistosomiasis. Recent commitments to donate treatments such as praziquantel, specifically for T. solium control have raised the possibility of augmenting these existing NTD programmes. We are currently assessing the additional impact of schistosomiasis control programmes in Uganda on T. solium, including the potential impact of additional praziquantel donations, which will provide insight into how effective this human-only strategy can be at a country-level, and whether a more comprehensive One Health strategy will be required to achieve the WHO NTD roadmap milestones.
The way forward
To address the challenge posed from a zoonotic infection the One Health approach uses a variety of strategies, such as:
- Understanding the complex system that maintains endemic infections
- Options for surveillance, control and elimination
- Structures for collaboration and sustainable financing
Adopting this approach for T.solium will hopefully provide a more collaborative way to sustainably tackle this persistent global health problem, and therefore improve the health and livelihoods of the communities affected by the disease.

Comments