
Soil-transmitted helminthiases (STH) are among the most common neglected tropical diseases (NTDs). Worldwide, it is estimated that 880 million children across 102 countries need treatment for these parasites. To eliminate morbidity from STH, the World Health Organization (WHO) recommends the periodical large-scale treatment of children in endemic areas.
Since 2010, this public health approach — also called ‘preventive chemotherapy’ (PC) — has been implemented and scaled up to impressive numbers. In 2018, more than 500 million children received medicine for STH.
This progress is being made possible thanks to an innovative public-private partnership, resulting in the largest medicine donation in history and tireless efforts by program managers, teachers and volunteers who support the implementation of annual targeted treatment of children at risk of STH.
In a new paper published in Infectious Diseases of Poverty, we show how sustaining preventive chemotherapy for at least 5 consecutive years leads to a decrease in STH burden in countries where data was available. Additionally, we show how monitoring the impact of control programs can be used to adapt strategies and reduce the need for medicine donations.
As the global STH community continues to scale up efforts and more countries sustain effective treatment coverage, the importance of impact assessments will increase and some challenges will need to be addressed.
Costs
Measuring progress of any infectious disease control program comes with an opportunity cost. The scarce public health resources available that are invested in measurement can also be used to enhance ground operations. On a global scale, measurements for the SDG indicator framework is estimated to cost from US$1 billion to US$1.25 billion per annum in the poorest countries alone.
This cost, however, forms only small part of the estimated US$3.5 and 5 trillion required annually to implement the Sustainable Development Goals (SDGs) globally. In addition, measuring progress in controlling NTDs through the SDGs, for example, can be used to highlight positive impact beyond its intended target. As we have shown, investing in measuring impact of STH control programs can reduce costs. Specific funds to measure the impact should therefore be included in financial plans of any STH program.
Tools
There are >40 HIV diagnostic tests pre-qualified by WHO, while only one STH diagnostic test forms part of the WHO’s Essential Diagnostics List. Though this test has limitations in terms of accuracy and ease-of-use, it is successfully being used to give an indication of disease burden and refine control strategies.
Nevertheless, the development of effective diagnostic tools for measuring STH burden continues to be an important avenue to pursue.
Reduction of drugs needed
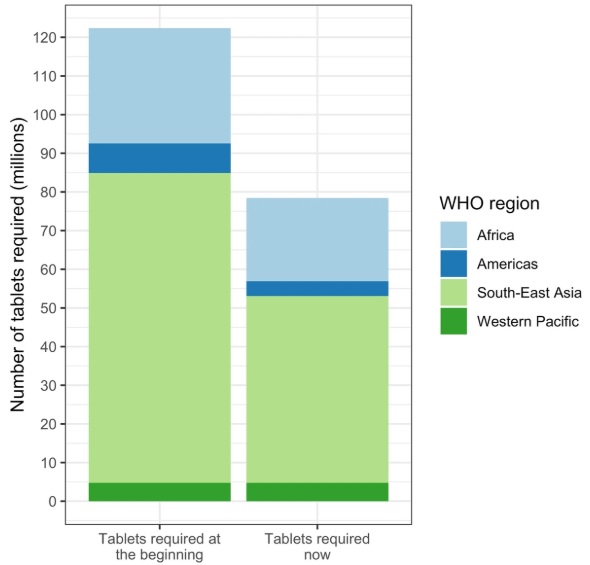
Even with these challenges, the countries assessed in our study were able to measure impact after sustained PC, and in some cases reduced the required frequency of interventions and the need for donated medicines by up to 36%.
Countries implementing PC should therefore periodically assess the impact of PC and adapt control measures to changing epidemiological situation, which can reduce PC costs and allow a move toward domestic financial support in order to sustain the fight against STH.
Importantly, the control of STH does not stop after sustained distribution of medicines. The NTD community needs to continue working with the WASH community, strengthen partnerships and mobilize resources to achieve a world where children don’t suffer from preventable NTDs.
The authors alone are responsible for the views expressed in this article and they do not necessarily represent the decisions or policies of the World Health Organization.

Comments