
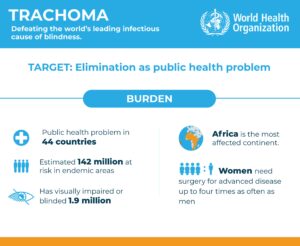
Trachoma is the leading cause of blindness due to an infection. Caused by the bacterium Chlamydia trachomatis, it affects marginalized and impoverished communities in 43 countries around the world. Trachoma spreads through personal contact, contaminated items, and by flies attracted to the eyes or nose of an infected person. Repeated infections lead to scarring of the inner eyelid, turning the eyelashes inward (trachomatous trichiasis (TT)) and causing excruciating pain and blindness if left untreated; this has resulted in the visual impairment or irreversible blindness of about 1.9 million people.
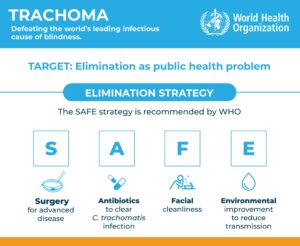
Despite being preventable and treatable, trachoma persists as a public health concern due to inadequate access to clean water, sanitation, and healthcare services in affected regions. Comprehensive strategies, including the WHO’s SAFE approach (Surgery, Antibiotics, Facial cleanliness, and Environmental improvement), are essential to combat this NTD. The disease has a wide distribution, disproportionately affecting the African Region, where 116 million people are estimated to be at risk. In addition to the terrible effects on the health of patients, trachoma also carries a heavy financial burden on individuals and their families as they are unable to work.
Fortunately, progress in disease control continues to be made, and just last year Togo became the third African country to be validated by the WHO for its elimination of trachoma as a public health problem.
Lessons learned
A recent paper by Bakoubayi and colleagues researches and reflects on the actions that led to this significant milestone for the country. In Togo, efforts to control trachoma began in 1989 with the establishment of the National Prevention of Blindness Programme (PNLC) under the Ministry of Health, Public Hygiene, and Universal Access to Care. In 2009, these efforts were integrated into the National Programme for Neglected Tropical Diseases (PNMTN), which prioritized trachoma, among other diseases. Control activities included screening for and managing late-stage trachoma complications (trachomatous trichiasis). Community health agents were trained to identify trichiasis cases during mass drug administration campaigns, and suspected cases were examined by ophthalmic nurses and provided with surgical correction.
Awareness campaigns promoting facial cleanliness and personal hygiene were conducted, and access to safe water and improved sanitation improved significantly. Population-based surveys played a big role in the surveillance of trachoma in Togo. They were conducted from 2006 to 2017, revealing the regions and districts with highest prevalence, allowing them to focus their activities where they were needed. In 2017, following WHO-recommended guidelines, a survey reported that the prevalence of key indicators fell below the thresholds set by the WHO. This demonstrating Togo’s capacity to identify and manage new TT cases within its health system.
The keys to success
Bakoubayi and colleagues describe how this achievement was the result of a close collaboration between multiple stakeholders, together with the affected communities:
- Political will was evident in the establishment of the National Program for Blindness control, which implemented the (SAFE) strategy recommended by WHO.
- The integration of trachoma control with other disease programmes was highlighted as a crucial action. This allowed activities like screening and door-to-door mass treatments to be done together with those for onchocerciasis, schistosomiasis, and geohelminthiasis.
- Community health workers played a crucial role in sensitising people and doing active case searching. Figures important to the communities were also engaged in these campaigns, including teachers, as well as administrative and religious authorities.
- The financial and technical support of international partnerships was also important in reaching this goal. This included support from WHO, the Center for Disease Control and Prevention, Sightsavers, Tropical Data and Health and Development International, and funding from the Bill and Melinda Gates Foundation and United States Agency for International Development.
A few bumps along the way
The authors are also mindful of the problems that can arise during such a long road towards elimination. One issue they mentioned is that changes in public health priorities and systems can affect the continuity and impact of control programmes. Another one they noted is that the surveys presented some methodological inconsistencies in the information collected between the different years. These are things to keep in mind for future public health campaigns.
The importance of continued surveillance
Since 2011, Togo followed the WHO integrated disease surveillance and response technical guidelines (IDSR), which uses indicator- and event-based surveillance to monitor public health events. Trachoma remains a part of the IDSR and is a notifiable disease, ensuring effective monitoring. Surveillance training for the detection of potential cases is carried out in key focal points, and community awareness campaigns for hand and face washing are still carried out every year. All these activities follow the examples set by other countries that have also eliminated trachoma, such as Oman, Morocco and Iran, and maintaining these will be essential in the years
The achievement of Togo in eliminating trachoma as a public health problem follows other successes also recognised by the WHO: the elimination of Guinea worm (2011), lymphatic filariasis (2017), and sleeping sickness (2020). Bakoubayi and colleagues finish their analysis by highlighting how this new milestone has improved the quality of life for many people in Togo living in previously endemic areas, and also emphasise the importance of sustained post-validation monitoring and surveillance.

Comments