
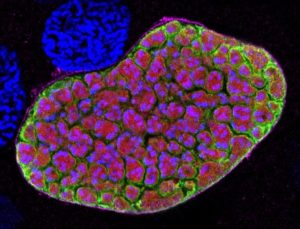
The malaria parasite develops through several stages in its human host. Initially, sporozoites, transmitted from mosquitoes during blood feeding, rapidly invade liver cells. Here they multiply asexually before they are released into the blood stream and go on to invade erythrocytes (red blood cells).
Clinical malaria is caused by the red blood cell stages whereas sporozoites and liver stage parasites do not cause disease symptoms.
Major advances in the elimination of malaria have been made this century, including the recent announcement that the WHO has declared China malaria free. This success has largely been achieved by control measures targeted at transmission of the parasite by mosquitoes, and by rapid diagnosis and treatment. However, progress towards the elimination of malaria from many other countries has been limited in the last decade, confirming the need for a highly efficient vaccine as the ultimate solution to eradicating this mosquito-borne disease. Of the five species of malaria infecting humans, Plasmodium falciparum is the deadliest, and this is the focus of attempts to produce an effective vaccine.
A promising concept being advanced currently is to target the pre-erythrocytic stages of the parasite, thus providing protection before any symptoms arise.
Pre-erythrocytic-stage vaccines
One approach has been to deploy a vaccine targeting an abundant molecule on the surface of sporozoites – circumsporozoite protein. This vaccine, named RTS,S and also known as Mosquirix, has been shown to provide short term protection to very young children in a Phase II trial involving over 12,000 children in African countries.
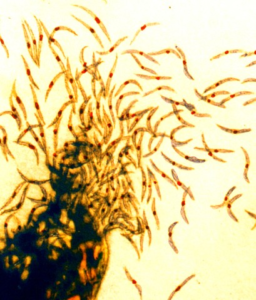
Another approach has been to inoculate with whole sporozoites that have been irradiated or genetically attenuated so that they invade the liver, but their development then stops. This would elicit an immunological response, but not cause clinical systems. This is the concept behind a vaccine developed by Sanaria Inc. of Rockville, Maryland, Sanaria PfSPZ vaccine. It has been shown, in laboratory based, controlled human malaria infections (CHMI) to give protection against the same strain of parasites as that used in the vaccine (homologous) and in the field, against different (heterologous) strains, but with reduced efficiency.
Using live unattenuated parasites
Sanaria’s latest vaccine developments have gone one stage further and their new vaccines contain live P. falciparum sporozoites that are still infectious. To prevent clinical malaria developing, the inoculation regime includes the administration of an anti-malaria prophylaxis. This is called a chemoprophylaxis vaccination (CVac). Using chloroquine, which kills parasites once they have entered the blood stream, they reported that the PfSPZ-CVac (CQ) vaccine gave good long-lasting protection against the same parasite strain as the homologous strain used in the vaccine, even at low doses.
It appeared that immune system exposure to blood stage parasites might be a requirement for the efficiency of this vaccine, but is there a possibility that parasites may escape the chloroquine treatment and lead to vaccination-induced infection?
Another concern was that the PfSPZ-CVac (CQ) vaccine did not appear to protect against heterologous strains. As there is a great variety of strains of P. falciparum worldwide, a marketable vaccine would need to protect against many strains.
A multi-author paper by Mwakingwe-Omari and colleagues, recently published in Nature, describes a further development that addresses these concerns.
Latest development
Their new experimental regime involved:
i) CHMI using their original vaccine, PfSPZ-CVac (CQ), or PfSPZ-CVac with a different prophylaxis, pyrimethamine, PfSPZ-CVac (PYR). Pyrimethamine kills parasites earlier than chloroquine, while they are still multiplying in the liver cells and before they enter the blood stream.
ii) Low and high vaccine doses were tested.
iii) The strain of malaria used to make these vaccines originated in West Africa. In the CHMI trials they challenged with this homologous stain, but also with a strain from Brazil (heterologous strain) that has a highly divergent genome, proteome and CD8 T cell immunome.
The previously demonstrated high level of protection given by PfSPZ-CVac (CQ) against homologous challenge was confirmed and, pleasingly, a four-fold increase in dose achieved 100% protection against the heterologous strain.
Increasing the vaccine dose also greatly improved the efficiency of PfSPZ-CVac (PYR), which reached 88% for homologous and 78% for heterologous CHMI challenge 3 months after vaccination. This level of protection was better than that reported using irradiated sporozoites and showed that exposure to blood-stage parasites is not required.
An immune response involving a subset of γδ T cell expansion was generated by both vaccines, and increased from the low to high dose of PfSPZ-CVac (PYR). This showed that antigens from liver-stage parasites are important initiators of immunity. Further investigations comparing these two vaccines could shed more light on the generation of an immune response by malaria parasites.
As expected, sub-patent parasitemia was detected by quantitative PCR (but not by microscopic analysis) in all PfSPZ-CVac (CQ) vaccinated participants and occurred before chloroquine could clear the parasites. The potential for break-through parasitemia could be problem in the field where compliance with the vaccination regime many not be 100%.
No parasitemia was detected in participants vaccinated with PfSPZ-CVac (PYR), as no parasites reached the blood.
What next?
The protection given by the PfSPZ-CVac (PYR) in these clinical trials is impressive and a field trial in Mali is now underway. Although the vaccination regime may be a difficult one to operate in the field due to compliance issues, the authors point out that pyrimethamine is widely used in parts of Africa as a prophylaxis and has an excellent safely profile. Scaling up sporozoite production (currently extracted from infected mosquitoes) to the number required to supply millions of doses would be challenging. However, the authors suggest this approach may prove suitable for travellers who visit Africa for a short period. They are most likely to comply with the vaccine regime of three doses and the accompanying drug treatment, and far fewer doses would be required than that needed to cover malaria-exposed populations.
In the future, a vaccine based on genetically modified parasites that live longer in the liver but are unable to enter the blood stream may be preferable as it would provide more exposure to the immune system than currently available GM parasites and remove the need for pyrimethamine treatment.

Comments