
BMC Infectious Diseases – Prevalence of covid-19 and long covid in collegiate student athletes from spring 2020 to fall 2021: a retrospective survey
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), responsible for COVID-19, has affected over seven hundred million people to date, leading to varied symptoms that can persist for weeks, months, or even years. Long COVID, officially termed post-acute sequelae of SARS-CoV-2 infection (PASC), poses unique challenges for athletes, impacting their physical, cognitive, and mental well-being beyond the acute phase of the virus. Despite its relevance, the prevalence of these prolonged symptoms remains unstudied among student athletes.
A study published in BMC Infectious Diseases delves into this issue, using surveys of 7,000 student athletes across 18 U.S. schools from spring 2020 to fall 2021.In spring 2020, 9.8% of student athletes tested positive for COVID-19, a figure that surged to 25.4% during the fall 2020 to spring 2021 academic year. Notably, 4% of those testing positive developed Long COVID.
This study contributes crucial data on COVID-19 and Long COVID prevalence among young, physically active individuals. A significant percentage of infections resulted in symptomatic cases, ranging from 25.2% to 79.6%, depending on the timeframe. Additionally, 1.0% to 4.3% experienced Long COVID, challenging assumptions about its rarity in young, healthy adults.
The survey underscores the substantial impact of COVID-19 on collegiate student athletes, emphasizing the need for further research to validate these estimates and address the diverse experiences of Long COVID among athletes. These findings carry implications for athlete well-being, guiding future public health measures and supporting targeted interventions for those grappling with the aftermath of SARS-CoV-2 infections in the athletic community.
 BMC Public Health – Finding your lane: experiences and beyond for adults learning to swim
BMC Public Health – Finding your lane: experiences and beyond for adults learning to swim
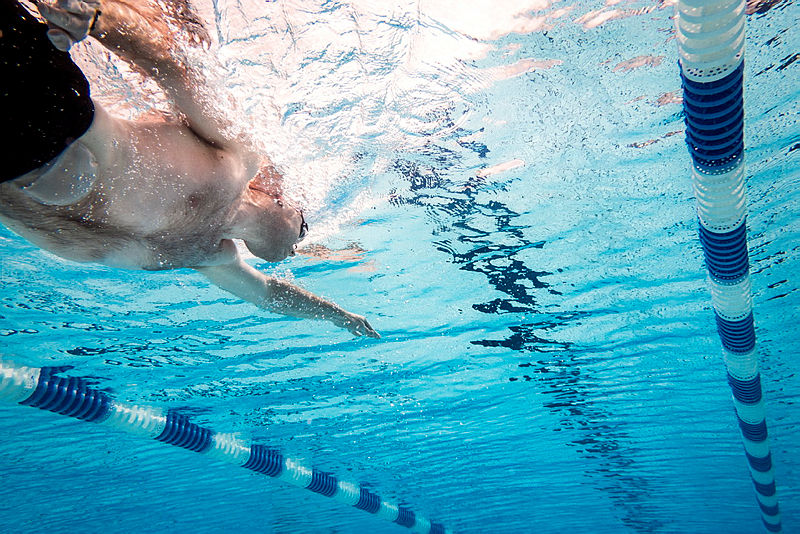
Aquatic activities offer a spectrum of benefits, including physical activity, social connections, and a sense of wellbeing. However, the lack of swimming skills poses a significant risk of drowning, affecting approximately 37% of U.S. adults. The limited research on how learning to swim can impact the lives of adults warrants the need to investigate the importance of adult swim instruction programs.
A study published in BMC Public Health reports on the barriers to swimming and discusses Knowles’ theory of adult learning to overcome these obstacles. The study focuses on the United States Masters Swimming Adult Learn to Swim (ALTS) program, designed to cater to adults interested in acquiring swimming skills. For the study, 20 semi-structured interviews were conducted, and the collected data was interpreted into three key themes: life affordance, emotional affect, and interpersonal relationships. Participants expressed how learning to swim not only provides a life-affirming skill but also opens doors to various water-based activities, enhancing overall wellbeing. Overcoming the emotional barriers tied to past negative experiences results in a transformational shift, with participants experiencing feelings of excitement, accomplishment, and increased confidence. Interpersonal relationships emerge as a significant motivator, with many adults inspired to learn due to family influences or their desire to ensure their own children can swim.
In conclusion, adult swim instruction programs extend beyond imparting swimming skills. They serve as catalysts for positive life changes, breaking down emotional barriers, fostering healthy relationships with water, and promoting overall well being. Recognizing these broader impacts is crucial for designing effective programs and addressing public health concerns related to drowning and limited swimming ability.
 BMC Digital Health – The effect of an adapted digital mental health intervention for sickle cell disease on engagement: a pilot randomized controlled trial
BMC Digital Health – The effect of an adapted digital mental health intervention for sickle cell disease on engagement: a pilot randomized controlled trial
Sickle cell disease (SCD), one of the most common genetic disorders, is characterized by the presence of abnormal sickle-shaped hemoglobin affecting millions of individuals worldwide. Individuals with SCD, particularly adolescents and young adults (AYA), face unique challenges that contribute to high risks of mental health disorders. Despite the prevalence of depression and anxiety in this population, they face barriers to traditional treatments such as a lack of accessibility and cultural relevance.
A study published in BMC Digital Health explores the potential of digital cognitive behavioral therapy (CBT) to address the mental health needs of AYA with SCD, especially in low-resource settings. To enhance the relevance of a digital CBT program, researchers made modifications such as incorporating Afrocentric and urban-themed images and creating a video highlighting shared experiences among individuals with SCD. The study enrolled 21 SCD patients from the University of Pittsburgh Children’s and Adult clinics in a randomized trial and compared a standard mental health app with an enhanced version of the app, tailored for minorities living with SCD. While overall engagement with the app was suboptimal, the group-specific adaptation showed promise, with participants in the enhanced group demonstrating greater engagement and improvements in pain, self-efficacy, and depression symptoms.
Despite the study’s limitations, such as a small sample size and challenges in participant engagement, it lays the groundwork for future research. The findings suggest that tailoring digital interventions for specific populations, like AYA with SCD, may be crucial for enhancing user engagement and treatment outcomes. The study underscores the potential of digital CBT as a scalable and accessible solution for addressing mental health disparities in vulnerable populations, urging further exploration and adaptation to meet the unique needs of those living with SCD.
 BMC Pregnancy and Childbirth – A repeated cross-sectional study of the association of community health worker intervention with the maternal continuum of care in rural Liberian communities
BMC Pregnancy and Childbirth – A repeated cross-sectional study of the association of community health worker intervention with the maternal continuum of care in rural Liberian communities
Comprehensive maternal care challenges persist in low- and middle-income countries, particularly in Sub-Saharan Africa, impacting maternal and neonatal health. The World Health Organization recommends specific care components, but limited access and completion rates prevail. In Liberia, a post-Ebola Community Health Assistant (CHA) program launched in 2016 aimed to enhance healthcare access showing significant improvements in childhood treatment and facility-based delivery through the National Community Health Assistant Program (NCHAP). However, its impact on the full maternal continuum of care was less known.
A study published in BMC Pregnancy and Childbirth assessed the association between NCHAP implementation and maternal continuum of care completion. The study utilized existing data from 2015, 2018, and 2021 collected from repeated cross-sectional household surveys of communities served by the CHA program in Rivercess County, Liberia. Rates of completing antenatal care, facility-based delivery, and postnatal care increased significantly post-implementation. Notably, the percentage of women receiving no steps in the continuum of care decreased remarkably. Factors influencing completion included distance from health facilities, wealth, and community accessibility. Living farther negatively impacted completion, emphasizing the program’s focus on reaching remote communities. Despite COVID-19 challenges, NCHAP demonstrated resilience, maintaining improved maternal care rates.
This study underscores the importance of community-based interventions, like the CHA program, in enhancing maternal care access. While achieving notable progress, there’s an ongoing need to address challenges for those living farthest from health facilities. These findings contribute valuable insights to inform and optimize future community-based initiatives, emphasizing the role of CHWs in reducing maternal and neonatal mortality.
Comments