
We have several anti-smoking policies in the UK in recent decades – the bans on indoor/workplace smoking, tobacco adverts around sports, and tobacco sales in vending machines, to name a few. Indeed, smoking has been the major target of public health interventions, and rightfully so given that it made the largest contribution to avoidable deaths. These public health interventions have been quite successful and, as a result, the number of smokers has been decreasing over the past 20 years.
With more people with obesity and fewer who smoke, it is now of question whether smoking remains the top contributor to UK’s deaths.
However, while smoking became less popular, we had more people with obesity. In 2003, 23% of people in England had obesity (BMI ≥30 kg/m2), and the number rises to 29% in 2017. Similar trends can also be observed in other nations in the UK. With more people with obesity and fewer who smoke, it is now of question whether smoking remains the top contributor to UK’s deaths.
We answered this question in our research by synthesizing two sets of numbers. The first set is the yearly proportions of people with different levels of obesity, and those of current, former, and never smokers. We extracted these numbers from the Health Surveys for England and Scottish Health Surveys. These surveys recruited random samples of people in England and Scotland, making their findings more representative.
The second set of numbers is what we called the risk ratios of obesity and smoking. Risk ratios quantify to which extent people with obesity and smokers are at higher risk of adverse health events, such as death. We extracted risk ratios from the latest meta-analysis studies, which should provide more robust estimates.
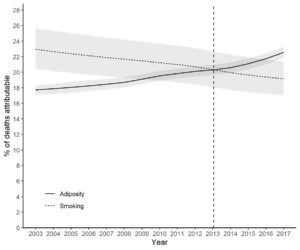
Combining these two sets of numbers, we found that smoking contributed 23% of all deaths in 2003, and that number decreased to 19% in 2017 (Figure). Meanwhile obesity contributed 18% deaths in 2003 and that number increased to 23% in 2017. The contribution of obesity exceeded that of smoking in 2013. The general trends were consistent across age, sex, and education level. But for younger people under 45 years of age, smoking remained the larger contributor to deaths.
It should, however, be noted that the analysis assumed the risk ratios could accurately reflect the extent to which obesity and smoking causes death over the 15 years. In addition, our study only considered deaths, but the impact of obesity and smoking extends to chronic illnesses and disabilities. The legacy of smoking, such as vaping, electronic cigarettes, and passive smoking, have also not been accounted for. These can be further investigated when better and more recent data are available.
Our analysis estimated obesity is now contributing to more deaths than smoking
Historical efforts to protect the public from the harms of smoking have been successful. Our analysis estimated obesity is now contributing to more deaths than smoking, which highlights the need to focus our efforts to address it. This could include government policies and legislation to create an environment that can facilitate weight management, as well as interventions to support individuals.
Comments