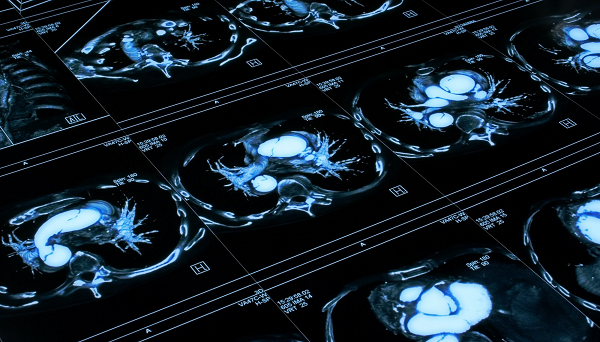
Cardiovascular mortality in end-stage kidney disease is much higher than the general population. The non-traditional risk factor of mineral bone disorders in this population plays an important role in the higher incidence of vascular calcification associated with an increased risk of cardiovascular disease and all‐cause mortality in this population. Several studies in hemodialysis patients have shown the advantage of using plain radiography to determine abdominal aortic calcification and cardiovascular disease. Cho et al. recently showed that abdominal aortic calcification score (AACS) is an independent risk factor for severe coronary artery calcification score on CT and predictor for cardiovascular disease in hemodialysis patients. Zhu et al. showed that abdominal aortic calcification is prevalent in hemodialysis patients and has the potential to predict cardiovascular mortality with use of plain radiography. There have not been similar studies in peritoneal dialysis (PD) patients.
A study by Ma et al., published this week in BMC Nephrology, sought to examine the predicative role of the AACS for major adverse cardiac and cerebrovascular events (MACCE) and mortality in PD patients. This study was a single-center, prospective, cohort study utilizing lateral lumbar radiography to determine the AACS for 292 PD patients. The patient population had a median PD duration of 28.4 months. One-fourth of patients had a history diabetes and one-third had a history of cardiovascular disease. The average AACS was 2.0. The patients enrolled were categorized into tertiles of low (meaning AACS = 0), medium (meaning AACS = 1-4) and high (meaning AACS > 4). The duration of follow-up averaged 43.6 months and there were 65 MACCE and 84 deaths. It was noted that the AACS was associated with age, PD duration, cardiovascular disease, and diabetes. Ma et al. observed that there was a significantly higher cumulative incidence of MACCE and all-cause mortality in the upper AACS tertile.
Should we routinely be getting plain radiographs for AACS in our end-stage kidney disease patients, especially our PD patients, based on this study and others?
Should we routinely be getting plain radiographs for AACS in our end-stage kidney disease patients, especially our PD patients, based on this study and others? I might strongly consider starting. An x-ray is a low cost, noninvasive test that could potentially help with risk stratification. Those patients with a high AACS should have immediate referrals to cardiology for cardiovascular disease prevention and evaluation. The frequency of testing and the initiation of testing would need to be clarified. Additionally, there is a potential use in kidney transplantation evaluations. Many transplant centers utilize a non-contrast CT as part of the transplant work-up addressing the site of anastomosis. Findings often prompt further cardiovascular disease testing. These CT results could help triage those who needed more extensive testing. Those with a high AACS might need to go directly to cardiac catheterization for diagnosis and treatment of cardiovascular disease. Whereas those with a low AACS might go directly to a stress test or coronary CT. This stratification could eliminate unnecessary testing, prevent complications, and save money.
The more passive approach would be using the information when abdominal aortic calcification is incidentally found. Then patients could proceed to a cardiology referral or further testing. However, in this population with a high incidence of cardiovascular disease and mortality, I would tend to take a more active role in prevention.

Comments