On September 20, 2017, the Category 5 Hurricane Maria made landfall on the U.S. territory of Puerto Rico. Maria left widespread devastation in its wake, with 95% of the island without electricity, half of the population without clean water, and much of the infrastructure, including the road network, destroyed. Even on October 6, two weeks after the event, the situation is largely unchanged, due to logistical difficulties compounded by the delayed federal emergency response. The 2017 Atlantic hurricane season proved to be a very active and devastating period that broke several records, such as being one in only six years featuring at least two Category 5 hurricanes. The first major storm was Hurricane Harvey that drenched Houston and parts of Louisiana with record amounts of rainfall of 64.58 inches. Following that, Hurricane Irma destroyed 95% of structures on the island of Barbuda, among other islands. Finally, Hurricane Irma devastated not only Puerto Rico but also the US Virgin Islands as well as Dominica.
When considering the potential effect of climate change on human health, most research has been concerned about the effect of increasing temperatures across the globe. These include dangerous heat waves, degrading air quality due to increasing ozone levels, as well as fine particulate matter from wildfires. In addition, increasing temperatures have been predicted to contribute to a potential range expansion of disease vectors, such as ticks, mosquitoes and sandflies, into novel regions, as well as increased likelihood of water-borne diseases. Some of these effects have already been observed, such as the expansion of Ixodes scapularis into Canada, as well as Vibrio parahaemolyticus outbreaks in Alaska and in the Baltic sea. However, there have been a lesser focus on the potential indirect effects of climate change on human health through the increased frequency and intensity of extreme climatic events, such as hurricanes.
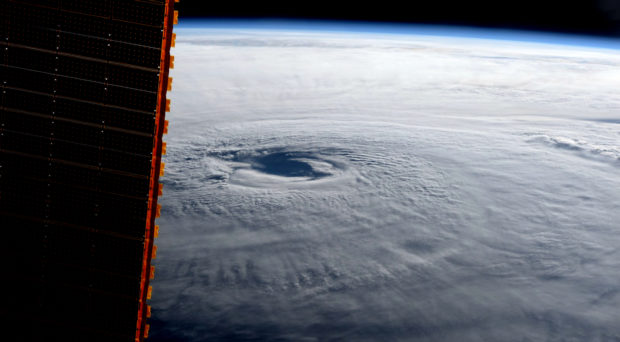
What does climate change have to do with the increased frequency and intensity of hurricanes? There are two distinct mechanisms for this association. We have already documented a sea level rise of 2.6 inches in 2014 above the 1993 levels, and it is continuing at a rate of 1/8 inch per year, due to the warming of the ocean as well as the melting of land-based ice. Increased sea levels lead to larger storm surge capacity as hurricanes and storms make landfall. Second, higher water temperatures increase the intensity of storms and hurricanes, and their frequency. Storms and hurricanes are like jet engines that use warm water as fuel, so the warmer the ocean is, the stronger they become. The intensity of these hurricanes then combine with the increased storm surge due to climate change, causing devastating results.
Hurricanes and other extreme events obviously cause massive devastation and economic harm. However, they also pose risk to human health, beyond the risk of physical injury. As these extreme events degrade existing infrastructure, specific populations become immediately vulnerable. Patients in ICUs in hospitals that lose power, or elderly at nursing homes without air conditioning, immediately become at risk. The flooding associated with these extreme events can subside very slowly, posing a series of health risks. Sewage systems flow backwards, contaminating streets and homes with potentially harmful bacteria. In hot and humid climates, molds grow very quickly on water-logged surfaces even as floodwaters recede. Residents can get infected with opportunistic pathogens while sustaining cuts and injuries during cleanup. Finally, remaining standing water provides ample breeding sites for mosquitoes. While the first mosquitoes arriving in massive numbers are usually flood-water mosquitoes that do not transmit specific pathogens, their sheer numbers can overwhelm, distract and impede recovery efforts. However, as floodwaters recede, accumulated debris provides a large swath of breeding sites for mosquitoes transmitting either dengue, Zika or West Nile virus.
In the absence of extreme events, residents in developed countries are protected from mosquitoes and the diseases they transmit partly simply by their lifestyle, with reduced exposure from not spending time outdoors as much and by having mosquito screens and air conditioning, as well as potted water and functioning sewage systems. This lifestyle requires a lot of infrastructure, such as electricity and piping. When these infrastructures become degraded in an extreme event, residents are at increased exposure risk to vector-borne diseases as well. In New Orleans, following Hurricane Katrina in 2005, a more than 2-fold increase of cases of West Nile Neurological Disease was reported. Large numbers of mosquitoes have been collected both after Hurricane Harvey in Texas as well as after Hurricane Irma in Florida, and mosquito-related calls surge after flooding events in general. Both Texas as well as Florida authorities resorted to aerial spraying campaigns to cut down their numbers. A similar risk is now apparent in Puerto Rico, which has a history of outbreaks of dengue fever as well as Zika virus. The newly formed Caribbean Emergency Vector Control Network has taken up the task of supporting islands in the region in terms of mosquito control and vector-borne disease prevention, and they are taking donations of equipment, supplies, insecticides as well as funds, and distribute that to affected islands.
In top of these concerns, the specter of cholera has been raised in Puerto Rico. The island has experienced three waves of large cholera outbreaks in the 19th century, which became important parts of local culture. While pathogenic Vibrio cholera species have not been detected in Puerto Rico since, a non-toxigenic strain of cholera has been found associated with the Mameyes River close to the capital of San Juan, which could have the potential to become pathogenic. While these concerns evoke images of the devastating cholera outbreak in 2011 in Haiti, we have to remember that that particular outbreak did not start until 8 month after the earthquake, when Nepalese UN peacekeeping soldiers introduced the pathogen. Hopefully, recovery efforts in Puerto Rico will restore the infrastructure quickly enough before such an introduction could take place. Rumors of cholera cases have already started spreading on Twitter, but these could not have been substantiated, and were refuted by informed professionals such as Maryn McKenna and Laurie Garrett. The CDC also tweeted that it is not currently concerned about an imminent outbreak of cholera on the island, and hopefully that will not change.
This years’ Atlantic hurricane season suggests that we might have seriously overestimated the structural resiliency of our existing infrastructure, and conversely underestimated the potential of extreme events to degrade it to a less developed state, which provides reduced protection to residents from infectious diseases. The question becomes whether our society will be able and willing to provide the resources (both material and human) to restore the infrastructure to its previous level before the next extreme event hits the same area. If not, we risk turning back to a less developed society where infectious disease risks of the past can reemerge. Ultimately, we need to transition our economies and society to renewable resources in order to impede the further acceleration of the frequency and intensity of these extreme events. In the absence of that, we either move away from their path, or adapt our infrastructure to the increased frequency and intensity of extreme events. I wonder which option would ultimately prove more costly in terms of money, human capital, and lives.

2 Comments