
Men’s grief following pregnancy loss and neonatal loss: a systematic review and emerging theoretical model.
What do we know about men’s experiences of grief following pregnancy/neonatal loss? And what are the factors/predictors that contribute to men’s grief? Philippa Middleton and co-workers in a paper published in BMC Pregnancy and Childbirth set out to answer these two questions by performing a systematic review of the existing literature.
The majority of previous research and subsequent pregnancy/neonatal loss bereavement care guidelines have focused primarily on the experiences and needs of heterosexual mothers. Fewer studies and recommendations relate to men’s experiences of grief and subsequent support needs. Given the potential for detrimental health and well being outcomes among men following pregnancy/neonatal loss, it is essential to further understand how men grieve, and the factors that contribute to worsened or improved outcomes.
The researchers identified 46 relevant studies investigating men’s grief following pregnancy/neonatal loss. By definition, this included the death of a baby at any stage in-utero, or up to 28 days after a live birth. Twenty-one studies investigated grief experiences following miscarriage (definitions which ranged between ≤20–24 weeks’ gestation), 10 following stillbirth, and 15 following a combination of loss types. Nineteen studies were quantitative, 26 qualitative and 1 was a mixed methods study. All studies were conducted in high-income countries, and male participants were heterosexual men who experienced pregnancy loss with a female partner.
The main findings of both quantitative and qualitative studies revealed the highly varied and individual nature of men’s grief. Although men’s grief was less intense compared to women’s in some quantitative studies, qualitative studies identified the significant impact of loss on men. In contrast to stereotypes that men intellectualize or rationalize their grief, studies also found that men do grieve on an emotional level. They may also oscillate between problem-focused coping and emotional expressions of grief, as reflected in the dual-process model of coping. However, men’s experiences also appeared to be consistent with the theory of disenfranchised grief, with a general silence surrounding pregnancy loss contributing to feelings of isolation and worsened grief.
The study also sought to identify predictors of grief. At an individual level there were mixed findings relating to demographic factors, suggesting that these have not been well-explored. Similarly, personality qualities may play a key role in predicting grief, although further research is required to confirm causality. However, in contrast to early assumptions that men only develop an attachment to the developing baby as gestation increases, the results suggested that attachment at any level is an important predictor of grief.
Men’s interactions with others seem to play a pivotal role in how they experience grief. The quality of the couple relationship contributed to either a positive source of support that helped the grief process, or a negative source of added stress which increased the impact of the loss. Grief was eased when friends and family were available to support men and were understanding of their loss. Furthermore, a positive experience with the healthcare system led to both reduced grief and increased support group participation, whereas insensitive treatment led to psychological distress and worsened grief.
There is an ongoing need for healthcare professionals to provide sensitive and empathetic care to both members of a couple. This includes adopting appropriate, jargon-free language, providing explanations relating to the cause of loss when available, and follow-up calls specifically to men in the weeks or months following a loss. Practical information on how best to support their partner, alongside recognizing and managing their own grief, was also desired by men.
Community attitudes concerning the legitimacy of parents’ grief following pregnancy/neonatal loss, along with gendered expectations relating to how men should behave in the face of loss, were also found to be important in shaping men’s experience. A lack of recognition for grief following pregnancy/neonatal loss resulted in disenfranchisement, with men frequently reporting a feeling of being overlooked as grieving fathers. Policies relating to woman-centered care and bereavement leave in the workplace also impacted grief. Where pregnancy was seen as an issue relating exclusively to women, and men consequently felt excluded from the loss experience at the hospital, their grief was worsened. A small number of studies also suggested that men were frequently not afforded adequate workplace leave to manage their grief following a loss. In line with recent investigations which have highlighted similar social and economic consequences of stillbirth, there is potential to re-examine current paternity and bereavement leave policies.
These findings suggest that individual-level supports should consider the above factors to provide tailored and appropriate support options to suit men’s individual needs. For example, individual counselling or support groups may not be appealing to all men. Rather, previous research has recommended creative options including activity-based supports, evidence-based online supports, opportunity for peer contact, or including male support workers in hospitals. The results also imply that beyond individual and interpersonal supports, there is also a need to educate the community about the impact of pregnancy/neonatal loss on men, as well as promoting their strengths to seek and accept, rather than avoid, support. The authors also suggest that strategies are needed to develop male-inclusive healthcare practices, and promote the meaningful engagement of men as equal partners throughout pregnancy and childbirth. In the broader postnatal health context, engagement of fathers has demonstrated improved long-term physical and mental health outcomes for women, men and babies.
Spontaneous embryo resorption in the mouse is triggered by embryonic apoptosis followed by rapid removal via maternal sterile purulent inflammation.
In normal development of mammals, a high percentage of blastocysts are lost before or after implantation by spontaneous resorption. Spontaneous resorption is a major problem in assisted reproduction in the human. Embryonic transfer (of two blastocysts) in the human results in a pregnancy rate of 30% and a “baby take home rate” of 21%.
Assessment of the occurrence of spontaneous resorption in early stages of pregnancy is challenging, especially in polytocous species. Resorption is very fast, so that with conventional methods only final haemorrhagic stages are encountered. Therefore, up to now it was impossible to foresee and to pick up spontaneous resorptions, which in the majority of cases occur shortly after implantation.
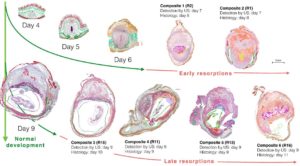
In order to overcome this problem Drews and co-workers in a paper published in BMC Developmental Biology aimed to identify the mechanism of spontaneous resorption in normal pregnancies. For this purpose, they analyzed by histology and immunohistochemistry 23 spontaneous embryo resorptions between days 7 and 13 of murine development. These were identified in a previous study by reduced growth rate and reduced heart rate in daily scans of pregnant mice with high-resolution ultrasound (US).
For histological description, the researchers grouped the specimens into early and late resorptions. The early resorptions were retrieved for histology at day 8 and the late resorptions between days 9 and 11. In the resorptions collected at days 12 and 13 only the placentae were preserved.
It was found that in the early resorptions detected at day 7, the embryo proper was replaced by maternal hemorrhage and a suppurate focus of maternal neutrophils. In the decidua maternal macrophages transformed to foam cells and formed a second focus of tissue dissolution.
In the late spontaneous embryo resorptions, it was found that the embryo undergoes endogenous apoptosis, which proceeds autonomously without maternal interference. During embryonic apoptosis caspase 3 is expressed and embryonic blood cells developed a macrophage like phenotype. Only when the foetal-maternal border breaks down and the innate maternal immune system comes in contact with apoptotic embryonic tissues, the mother mounts a sterile unspecific inflammation and the apoptotic embryo is aborted into the uterine lumen and rapidly resorbed. Failure of lacunar trophoblast and dissolution of the decidua capsularis in the resorptions were clearly discernible from physiological involution of these structures in the normal littermates at days 10 and 11. Rupture of the embryonic vesicle and abortion were accompanied by maternal hemorrhage and massive invasion of maternal neutrophils. The maternal part of the implantation site dissolves by apoptotic liquefaction and transformation of F4/80 positive macrophages into foam cells.
Studies like the above help us increase our understanding about the mechanisms of spontaneous resorption in normal pregnancies and bring us closer in identifying points of intervention to maximize success rates of normal pregnancies and in vitro fertilization.
Post-traumatic stress disorder and risk of selected autoimmune diseases among US military personnel.
 Posttraumatic stress disorder (PTSD) is a psychiatric disorder that can result from experiencing or witnessing a traumatic event, such as a serious accident or violent assault. Compared to the general population, military personnel are often exposed to dangerous situations and traumatic events, and therefore are at higher risk for mental disorders.
Posttraumatic stress disorder (PTSD) is a psychiatric disorder that can result from experiencing or witnessing a traumatic event, such as a serious accident or violent assault. Compared to the general population, military personnel are often exposed to dangerous situations and traumatic events, and therefore are at higher risk for mental disorders.
Individuals with PTSD remain in a perpetual state of hyperarousal and fear. As such, PTSD is associated with endocrine, immune, and neurobiological abnormalities. Posttraumatic stress has been shown to impede functioning of the hypothalamic pituitary adrenal axis, the autonomic nervous system, and the immune system. Specifically, lower levels of glucocorticosteroids, elevated proinflammatory factors, altered gene expression, and accelerated aging of immune cells may lead to immune dysfunction that underlies the pathogenesis of multiple immune-mediated inflammatory diseases. Furthermore, interactions within the neuroendocrine system are bidirectional, meaning that hyperarousal and subsequent increased hormonal activity in the central nervous system can trigger the release of excess levels of stress hormones that further contribute to chronic immune dysregulation and the potential development of autoimmune disease.
Findings from previous studies indicate that there is an association between PTSD and autoimmune diseases, however, these studies were restricted to veterans after the end of their military service, civilian populations, or to a single gender. Moreover, little is known about the potential role of combat and sexual assault in relation to PTSD and autoimmune disorders. Given the relatively young age at onset for many autoimmune diseases and the high prevalence of PTSD in the military, current military members comprise an important population in which to investigate risk of autoimmune disease in relation to PTSD and better understand the role of specific traumatic events.
A study by Rudolph P. Rull and co-workers published in BMC Psychology prospectively examined the association of PTSD and risk of several relatively common autoimmune diseases, including rheumatoid arthritis (RA), systemic lupus erythromatosus (SLE), multiple sclerosis (MS), and inflammatory bowel disease (IBD). The study population was 123,761 participants who were serving on active duty when they completed the baseline survey. Data was gathered from the Millennium Cohort Study, a large cohort of US service members. Approximately 71% of the population was male while the baseline prevalence of PTSD was 8% among men and 9% among women. At baseline, both men and women with a history of PTSD were more likely than those without PTSD to be younger, of enlisted rank, in the Army, a current smoker, a heavy or problem drinker, or obese. Those with PTSD were also more likely to have a history of another mental health condition, combat experience, or physical or sexual trauma. Prior combat experience was more common among men, whereas prior physical or sexual trauma was more common among women.
During a mean follow-up of 5.2 years (SD, 3.7 years), 864 participants (55% men, 45% women) were identified with the autoimmune diseases of interest (309 RA, 103 SLE, 151 MS, and 332 IBD). Incidence rates for RA, SLE, and MS were higher for women than for men, whereas rates were similar for IBD. For the composite outcome of any of the selected autoimmune diseases, risk was higher for those with a history of PTSD relative to those with no PTSD in a multivariable model adjusted for demographics and history of another mental health condition. The relative risk for a history of PTSD for each individual autoimmune disease ranged between 1.4 to 2.3 times that of those without a history of PTSD, though estimates were least precise for SLE and MS. Effect estimates stratified by sex did not differ appreciably except for MS and IBD, but estimates were generally imprecise. Further adjustment for BMI, smoking status, and alcohol use did not appreciably change the magnitude of each effect estimate.
To sum up, although estimates for each individual autoimmune disease were generally imprecise, there was an approximately 60% increased risk for the composite outcome of any of the selected autoimmune diseases —RA, SLE, MS, and IBD—for those with a history of PTSD relative to those without a history of PTSD. The magnitude of this association did not materially differ between men and women, though as expected absolute incidence rates were generally higher among women. In addition, findings did not differ according to specific types of prior trauma and healthy behaviors did not appear to influence this association between PTSD and autoimmune disorders.
The findings from this analysis contribute to an emerging body of evidence that suggests that PTSD may be a risk factor for autoimmune disease. Furthermore, it was observed that the magnitude of this association appears to be similar among those with and without a history of specific traumatic experiences such as combat exposure and physical or sexual trauma. The present study suggests that further research is needed to understand the underlying biological mechanisms which may link PTSD with increased risk of immune-mediated inflammatory conditions, as well as how severity of PTSD may link with increased autoimmune disease risk or severity of illness, and understand whether successful treatment of PTSD may mitigate the risks of these non-neuropsychiatric complications.
“I just keep thinking that I don’t want to rely on people.” a qualitative study of how people living with dementia achieve and maintain independence at home: stakeholder perspectives.
 The number of people living with dementia worldwide is set to triple from over 46 million to 131.5 million by 2050. Dementia profoundly impacts upon the person living with dementia, their family and carers and wider society. Most people diagnosed with dementia wish to continue living in their own homes as independently as possible, however with progressive functional dependence, this can be difficult.
The number of people living with dementia worldwide is set to triple from over 46 million to 131.5 million by 2050. Dementia profoundly impacts upon the person living with dementia, their family and carers and wider society. Most people diagnosed with dementia wish to continue living in their own homes as independently as possible, however with progressive functional dependence, this can be difficult.
For people living with dementia, there can be a tension between independence as an expression of autonomy and interdependence enabling people with dementia to remain in their own homes and communities. Qualitative research has explored the ethical dilemmas faced by family carers and professionals in promoting the dignity and autonomy of people living with dementia and deciding how best to adapt the home environment to facilitate independence. However, less is known about how people living with dementia, family carer and professional perspectives differ. This knowledge is important in order to inform the development of psychosocial interventions to enable people with dementia to live well for longer at home.
The study by Claudia Cooper and co-workers in BMC geriatrics is the first qualitative study to explore how people living with dementia, family carers and health and social care professionals understand independence at home for people living with dementia. The researchers conducted an inductive thematic analysis of qualitative interviews with 11 people living with dementia, 19 professionals and 22 family carers in England. Participants were recruited in urban, semi-rural and rural areas, were of both genders and of differing ages, ethnicities, nationalities and experiences. Four overlapping themes were identified: Being in a safe familiar environment, enabling not disabling care, maintaining relationships and community connectedness and getting the right support.
Stakeholders agreed that a person-centred approach prioritizing the inherent value of all people with dementia, seeking to uphold rights and promote abilities was important. Professionals often perceived such an approach as being relatively straightforward, while family carers and people living with dementia pointed to a myriad of ethical and practical dilemmas. For family carers these dilemmas often linked to the perceived safety of their relative and the family carer’s sense of personal responsibility. For people with dementia, the act of accepting support was paradoxically both an outward sign of dependence and an enabler of independence. Concepts such as relative interdependence, delegated autonomy and social and spatial independence have previously been applied to understanding independence in older people living in a range of residential settings. These concepts feel especially relevant to the nuanced and complex experiences of people living with dementia and those caring from them and the dynamic nature of interactions and negotiations around independence discussed in this paper.
These findings highlight the relational nature of independence at home: the dynamic interaction between the person living with dementia, the family carer and professional support, situated within a resource-limited, wider societal context. Professionals were responding to ‘living well with dementia’ or ‘dementia positive’ agendas, perhaps underestimating the complexity and textured nature of the lived experiences of family carers and people with dementia themselves. Professionals promoted positive risk taking whereas family carers felt they were left holding this risk or persuading relatives to act in a particular way. For people living with dementia the realities of getting into the community and playing an active part were far from straightforward. Psychosocial interventions must accommodate tensions between positive risk-taking and avoiding harm, facilitating autonomy and providing support. They should be adaptive and collaborative, combining self-management with flexible support and consider the emotional burden for family carers of supporting someone to live positively with risk.
Potential impacts of a novel integrated extracorporeal-CPR workflow using an interventional radiology and immediate whole-body computed tomography system in the emergency department.
Extracorporeal cardiopulmonary resuscitation (ECPR) can restore blood circulation in patients with out-of-hospital cardiac arrest (OHCA), as the cardiopulmonary circuit allows immediate stabilization via effective perfusion and gas exchange. ECPR devices are becoming smaller and cheaper, providing an opportunity to install this rescue therapy in the emergency department (ED). The International Resuscitation Guidelines mentioned ECPR as a potential support to be considered in settings where it can be rapidly implemented, and for selected patients with a suspected etiology of cardiac arrest that is potentially reversible with immediate mechanical cardiorespiratory support. However, there remains insufficient evidence to recommend the routine use of ECPR for patients with OHCA.
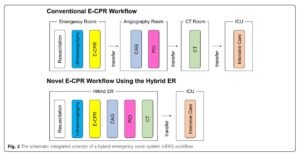
A novel integrated trauma workflow concept that utilizes a sliding computed tomography (CT) scanner and interventional radiology (IR) system, named a hybrid emergency room system (HERS), allowing emergency therapeutic interventions and CT examination without relocating trauma patients, has recently evolved in Japan. HERS can drastically shorten the ECPR implementation time and more quickly facilitates definitive interventions than the conventional advanced cardiovascular life support workflow. In this paper published in BMC Cardiovascular Disorders, Satoshi Fujimi and co-workers discuss a novel workflow concept using HERS on ECPR for patients with OHCA that can drastically shorten the ECPR implementation delay and more quickly facilitate definitive interventions than the conventional workflow, without relocating the patients.
The authors previously demonstrated that the HERS is associated with a decreased mortality in patients with severe blunt trauma compared to that with conventional trauma management, even after accounting for potential confounders. Patients treated with the HERS had shorter time intervals from ER arrival to CT examination and emergency surgery compared to those for conventional management. These beneficial observations contributed to the rapid spread of the HERS concept; as of September 2019, eleven tertiary emergency hospitals in Japan and one trauma center in Korea have installed a HERS. This system could be well adapted to ECPR, providing an expedient initiation of mechanical cardiopulmonary support for patients with non-traumatic OHCA. Immediate high-quality CPR, providing effective oxygenation to the vital organs until return of spontaneous circulation (ROSC) is achieved, is crucial for optimal outcomes. However, there is no consensus regarding the CPR time interval before ECPR implementation.
Yannopoulos and colleagues previously evaluated a novel protocol with early transport to a cardiac catheterization laboratory (CCL) for ECPR and revascularization in OHCA patients with refractory ventricular fibrillation/ ventricular tachycardia. In patients who received the early transport protocol, the average time from the 911 call to CCL arrival was 58 ± 17 min, 28/62 (45%) patients survived to hospital discharge, and 26 (42%) had functionally favorable outcomes. In contrast, only 26/170 (15.3%) patients in a historical routine care group survived to hospital discharge with a favorable outcome. These observations suggest that, in these patients, the early initiation of ECPR to allow for coronary angiography (CAG) and percutaneous coronary intervention (PCI) would likely be more effective than continuing non-invasive conventional advanced cardiovascular life support (ACLS) alone.
The schematic concept of HERS integrated workflow the authors propose is described in Fig. 1. The HERS enables ACLS to be followed seamlessly by ECPR induction and post-ECPR procedures, including CAG and PCI, without any patient transfer. The HERS likely shortens the time from the 911 call to ECPR initiation and improves survival in OHCA, as early transport contributes to improved outcomes. In addition, the HERS enables safe head and body CT examinations during the post-ECPR phase, even in hemodynamically unstable patients, while in-hospital transport with an extracorporeal membrane oxygenation (ECMO) device implantation can cause considerable harm. Thus, given that an extremely time-conscious algorithm should be adopted in the management of, not only severe trauma but also life-threatening critical illnesses mentioned above, the HERS can provide benefits for cardio-cerebral resuscitation in patients with OHCA or severe medical conditions.
Comments