
What is psoriasis?
Psoriasis is a chronic, inflammatory condition, which affects the skin’s surface. The condition causes inflamed, red, flaky and itchy skin, often around the knees, elbows and scalp. The condition is believed to affect 1 in 50 people, affecting all ages, races and genders. A large percentage of people are diagnosed below the age of 35. Currently, it is thought that psoriasis affects roughly 100 million people worldwide, 1.6 million in the UK and nearly 7.6 million Americans, making psoriasis a global problem.
Psoriasis lesions are often located in areas of the body that are visible to other people. Despite being fairly common, there are often misconceptions that the condition may be contagious and is known to affect people’s self-esteem. Since the condition is chronic, this can negatively impact the mental health of people experiencing the condition. The National Psoriasis Foundation (NPF) notes that depression is the number one comorbidity of psoriasis. People with psoriasis are twice as likely to become depressed as the rest of the population.

In popular culture, businesswoman and television personality, Kim Kardashian, has recently announced she experiences the condition. Given Kardashian’s huge social media following, it is possible that this could help to bring awareness to the condition and comfort and understanding to those who also experience psoriasis.
What do we know about psoriasis?
The National Psoriasis Foundation (NPF) notes that depression is the number one co-morbidity of psoriasis.
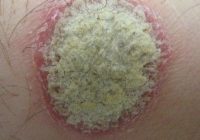
Although psoriasis is common, the condition is under-researched. The underlying cause of psoriasis is thought to be our immune system unnecessarily accelerating the growth of skin cells resulting in inflammation. It is thought that combinations of genes as well as exposure to particular external factors are likely to trigger development of the condition. Scientists have now identified about 25 genetic variants, which increase the probability of a person developing psoriasis. The most common form of psoriasis, plaque psoriasis, is thought to be caused by a rare genetic mutation known as CARD14. Stress, weather changes, medications, infections, skin trauma, smoking and alcohol are all thought to flare up the condition. Most people experience small lesions, however, severity varies on a case-by-case basis. The condition is split into six main types; plaque psoriasis, scalp psoriasis, guttate psoriasis, pustular psoriasis, psoriasis in sensitive areas and nail psoriasis (summarized in table 1).
| Type | Area affected | Description |
| Plaque Psoriasis | Whole body | The most common type of psoriasis. Caused by a build-up of skin cells known as ‘plaques’. |
|
Scalp Psoriasis
|
Scalp | May result in dandruff like flakes and in extreme cases cause thinning of the hair. |
| Guttate Psoriasis | Torso back and limbs | Also known as ‘tear drop’ psoriasis due to the shape of the spots that are often bright pink or red on the skin. |
| Pustular Psoriasis | Whole body | Results in small white or yellow blisters on top of red or darkened skin. The blisters are often filled with fluid giving them a yellow colour. |
| Psoriasis in Sensitive Areas | Face, armpits genitals and skin folds. | Skin is more sensitive in particular areas, especially around skin folds / clothing. |
| Nail Psoriasis | Nails | Often affects the nails or toenails and can be painful, restricting movement. |
Table 1: Summary of the different types of psoriasis
Despite being fairly common, there are often misconceptions that the condition may be contagious and is known to affect people’s self-esteem.
The severity of the condition is assessed by the Physician Global Assessment (PGA) scale, which is a 6-point, 0-5 measure of psoriasis based on different symptoms, across the whole body. It is used to standardize the diagnosis of psoriasis, particularly in clinical trials.
A recent article published in BMC Dermatology collected data from 3641 patients suffering with moderate, severe and chronic psoriasis. A version of the PGA scale was applied to participants in a clinical trial setting, to test its validity. The study provided an ‘intensive and rigorous’ analysis of the scoring matrix. It concluded that the scale is reliable to obtain a global assessment on the severity of psoriasis, further validating the three-item PGA tool.
What treatments are available?
Currently, there is no permanent treatment available for psoriasis. Initially, treatment often involves topical creams applied to the skin to help relieve the symptoms of the condition. Treatments vary on the type and severity of psoriasis.
Scientists are working on new treatments for the management of the condition. This includes the use of a therapeutic antibody, or monoclonal antibody, called Secukinumab. Two proteins involved in human immune responses, Interleukins 12 and 23, have been suggested to play a role in the development of psoriasis. Therefore, researchers have developed a human monoclonal antibody to disable these proteins.
A study protocol recently published in BMC Dermatology lays out the plans to assess the real world safety and effectiveness of Secukinumab in the management of moderate to severe psoriasis through a multinational study. Previous controlled clinical trials have shown Secukinumab to be safe and effective and the results of this up-and-coming trial hope to highlight the real world, long term benefits of Secukinumab, in turn improving quality of life in patients with moderate to severe psoriasis.
Comments