
The value 3D printing offers for surgical planning of complex canine surgeries is demonstrated in a recently published case series in 3D Printing in Medicine. Dr. Yu-Hui Huang and Dr. Stephanie Goldschmidt share how the collaboration between radiology and veterinarian medicine was fostered through the care of Dr. Huang’s own dog, Chubbs.
During Dr. Huang’s clinical anaplastology training, she assisted in virtual surgical planning and 3D printing of patient specific anatomical models and surgical guides for craniofacial surgeons. Dr. Huang saw first-hand how the technology could be utilized to enhance personalized medicine and improve patient outcome. When Dr. Huang’s 9-year-old English bulldog, Chubbs, was diagnosed with maxillary chondroblastic osteosarcoma, she thought to do the same for Chubbs.
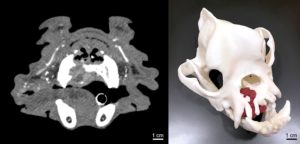
After obtaining Chubbs’ contrast enhanced computed tomography (CT) from Dr. Stephanie Goldschmidt, the veterinary surgeon, Dr. Huang was able to segment his skull and tumor using 3D Systems DICOM to Print (D2P), an FDA-cleared segmentation software. She first printed the skull with the tumor using her Formlabs Form 3B printer via vat photopolymerization technology. To facilitate anatomical and tumor visualization, she hand-painted the tumor red while referencing his CT data.Thanks to the collaborative generosity of the Minneapolis VA Minneapolis Adaptive Design & Engineering Program (MADE), Chubbs’ skull was also printed using a Stratasys J750 with material jetting technology which allowed for the skull and tumor to be printed in white and magenta, respectively.
Through Chubbs, a meaningful collaboration was fostered.
Visualization and tactile assessment of tumor extent on the 3D printed model by Dr. Goldschmidt led to the conclusion that curative intent surgery with 2 cm margins would carry a high risk of potential morbidity. Therefore, it was elected to excise the tumor with conservative margins (0.5-1 cm) and treat with postoperative radiation therapy to minimize potential complications. Chubbs did remarkably well for over a year after his surgery and adjuvant radiation therapy.
Through Chubbs, a meaningful collaboration was fostered, where Dr. Huang was able to assist Dr. Goldschmidt with 3D printing anatomical models and biocompatible surgical guides for other complex canine oral and maxillofacial surgeries.
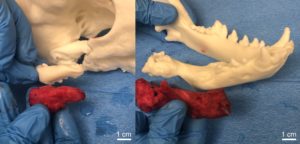
The next patient was an 8-year-old male Boston terrier with plasma cell tumor, causing osteolysis of his rostral mandible, requiring surgical reconstruction. Using his preoperative cone beam CT (CBCT), Dr. Huang was able to segment and print his skull via vat photopolymerization. The 3D printed skull model was utilized for preoperative planning and served as an intraoperative reference for bilateral rostral mandibulectomy and pre-contouring of the titanium plate for mandibular reconstruction. By allowing pre-contouring of the titanium plate, the printed model was estimated to decrease surgical time by approximately 30 minutes. As of 4 months post-op, the Boston terrier is doing well with bony consolidation demonstrated on his follow-up CBCT.

Our final patient described in the case series was a 6-month-old male Labrador retriever who presented with severely decreased range of motion secondary to recurrent temporomandibular joint (TMJ) ankylosis post gap arthroplasty. Joint ankylosis developed secondary to a dog bite that occurred at 8 weeks of age. Initial gap arthroplasty was performed 10 weeks after the trauma due to a progressive decrease in range of motion. Approximately 3 months following the initial surgery, the range of motion began to progressively decrease again, and it was confirmed by CBCT that there was new bone formation with subsequent ankylosis.
As 3D printing technology continues to advance, there will be increased adoption in veterinary medicine
Due to the increased complexity of the surgery, anatomical models and surgical guides were designed and fabricated via vat photopolymerization. The skull model was printed in white resin and a surgical guide was fabricated in biocompatible surgical guide resin. The 3D printed skull and surgical guide were sterilized to serve as intraoperative reference and guidance for the gap arthroplasty and osteotomies. The 3D printed models and guide are estimated to have saved up to an hour of operation and anesthesia time by allowing the surgeon and trainee to have a tactile appreciation of the lesion and thus be more confident in operating in a very high-risk location.
Since the publication of our case series, we have continued to utilize 3D printing to assist in the clinical care of both veterinary and human patients. 3D printed models can improve preoperative planning and intraoperative guidance while enhancing healthcare/veterinary training and patient/pet owner communication. As 3D printing technology continues to advance, there will be increased adoption in veterinary medicine as it is already evidenced in human medicine with more hospitals offering medical 3D printing. We aim to continually refine, validate, and improve our workflow while collecting more outcome-based evidence on the utilization of medical 3D printing for our patients with complex needs.
Comments