
Have you ever had low back pain? If not, you probably know someone who has. About 80% of the population will experience at least one episode of low back pain in their life. Although in most cases the problem is resolved within a few weeks, pain flare-ups are common and some people will develop chronic low back pain (i.e. when the pain persists for more than 3 months).
Chronic low back pain is a heterogeneous condition. For some people, mainly psychosocial factors (e.g. fear of movement) contribute to the persistence of their back pain. For others, physical factors (where the pain is closely linked to mechanical loading of the spine), are more significant, meaning that the pain is typically provoked or eased by certain postures or movements.
When people have to learn new movement skills, it is essential that they receive feedback about their performance in order to correct themselves.
To illustrate the latter, consider the following example: Claire complains about low back pain when she sits for a while, has to lift objects, and when she puts on her socks in the morning. On examination, we can see that Claire always tends to flex (i.e. bend) her lower back excessively during these activities. Limiting the exaggerated flexion reduces her pain.
To improve Claire’s problem, we can use movement control exercises. The aim of these exercises is to learn how to control movements into the painful direction, thereby reducing the mechanical load on the painful structures. In Claire’s case, this would mean that she has to learn to bend less in the lower back and move more in an adjacent joint, such as the hip.
When people have to learn new movement skills, it is essential that they receive feedback about their performance in order to correct themselves. Because a physical therapist is not always present to provide feedback, patients with low back pain frequently perform exercises in front of a mirror so they can watch the movements of the spine. Without experience, however, it is often difficult to accurately assess spinal movement in a correct way. As such, a mirror might not be the most effective tool for providing feedback.
Improving feedback with new technologies
With the development of rehabilitation technologies, new opportunities for providing feedback have emerged. For example, wireless motion sensors can be used to provide easy-to-understand and accurate feedback to the patient.
Therefore, we asked ourselves whether sensor-based feedback would be more effective than mirror feedback for improving movement control. We investigated this by conducting a randomized controlled trial in patients with chronic low back pain.
At baseline assessment, participants performed two movement control tasks, during which the range of motion in the lumbar spine (lower back) and hip joint were measured. First, participants performed a lifting task. They were asked to lift a box while maintaining their lumbar curvature, i.e. not to flex or extend the lumbar spine (Fig. 1A). Thereafter, participants performed a waiter’s bow. During this task, participants stood with slightly flexed knees. They were then asked to bend forward in the hips, while maintaining their lumbar curvature (Fig. 1B). The tasks were standardized for participants’ height.
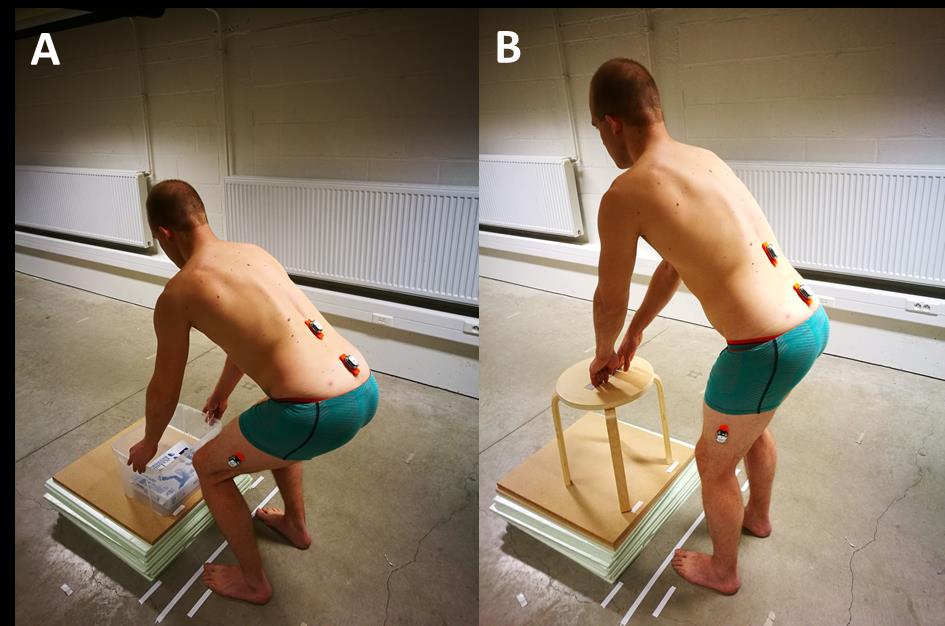
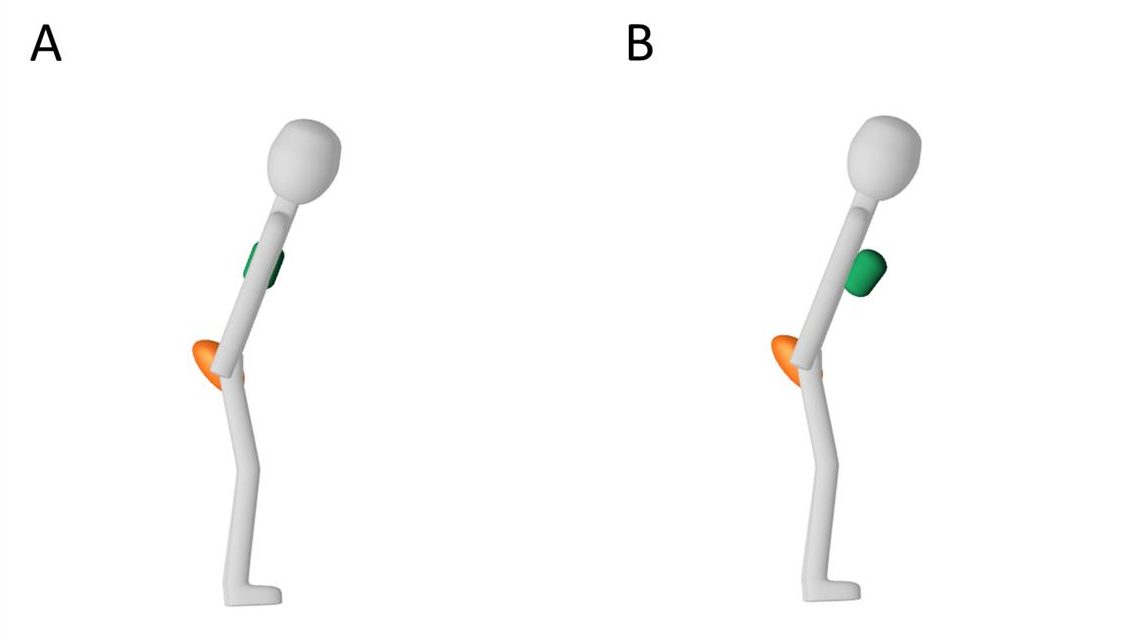
After baseline assessments, participants were randomized into three subgroups. During the intervention, each subgroup received a different type of feedback, i.e. feedback from movement sensors (Fig. 2), from a mirror, or no feedback (control group). The intervention consisted of a single exercise session of 18 repetitions (3 sets of 6 repetitions), during which participants practiced the waiter’s bow. The lifting task was not practiced. Immediately after the intervention, the baseline assessments were repeated.
We found that the movement control of participants in the sensor-group improved significantly more compared to those in the mirror and the control groups. This means that they were able to bend more in the hips, and less in the lumbar spine.
These improvements were present during the waiter’s bow and the lifting task. This indicates that participants in the sensor groups were able to transfer their newly learned movement skills from a practiced (waiter’s bow) to a non-practiced (lifting task) movement.
The current study shows the potential of sensor-based feedback for improving movement control in patients with chronic low back pain. Future studies should investigate whether these improvements persist in the long term, and whether practicing exercises with sensor-based feedback leads to larger improvements in pain and disability compared to conventional exercise therapy.
Comments