Neoepitopes derived from tumor-specific mutations are promising targets for cancer immunotherapy. While neoepitopes have been widely explored in adult cancers, the potential for targeted therapies based on neoepitopes in childhood cancers has so far remained uncertain.
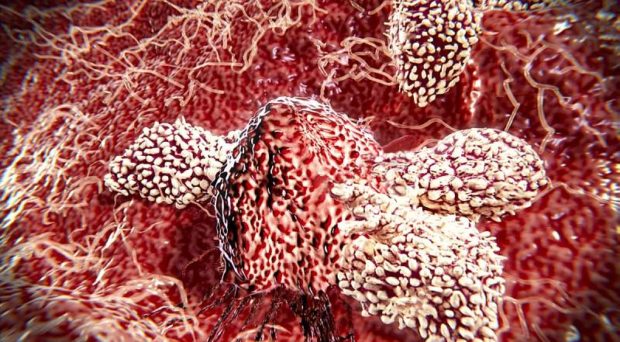
Our recent study identifies neoepitopes that could be targets for childhood cancer immunotherapy. Neoepitopes present on tumor cell surface are recognized by T cells, which carry out tumor-specific immune responses. As such, neoepitopes can be used to prompt T-cells to destroy cancer cells, which makes them promising targets for the development of tumor vaccines or other types of T-cell based immunotherapy. Neoepitopes can be synthesized and packed into custom-made vaccines to produce a tumor-destroying immune response in patients. Alternatively, T cells targeting neoepitopes can be transferred into patients for treatment.
Identifying neoepitopes from mutations
Many cancers arise from mutations in genes that regulate cell division or that play a role in important processes like DNA damage repair.
By comparing DNA sequences between normal and cancer cells, we were able to identify cancer-specific mutations that cause genes to produce new versions of proteins or peptides – otherwise known as neoepitopes.
Evidence from our study indicates that tumors with defects in DNA damage repair possess an increased number of mutations and neoepitopes
One of the challenges of neoepitope-based immunotherapy is how to efficiently select neoepitopes that prompt an immune response. Recent advances in DNA/RNA sequencing technology and improvement of epitope prediction algorithms allowed us to develop a data analysis method that predicts neoepitopes in 23 subtypes of childhood cancers. The analyses were based on mutated peptides resulting from genetic mutations as well as gene fusion events in cancer cells, by which a part of one gene combines with another.
Our analyses revealed that a large fraction of childhood cancers harbors mutations that generate specific neoepitopes. Several neoepitopes were identified from mutation hotspots – genomic positions that are mutated frequently. We also demonstrated that gene fusions can generate neoepitopes in multiple types of childhood cancers, including leukemias.
Mutation rates vary across tumors and recent studies have shown that tumors with a high mutation rate, such as melanoma, have a higher number of neoepitopes than other tumor types. This leads to a hypothesis that tumors bearing more mutations are likely to be more responsive to immunotherapy.
Evidence from our study indicates that tumors with defects in DNA damage repair possess an increased number of mutations and neoepitopes. This subset of cancers, which include childhood high-grade gliomas, may have an enhanced antitumor response to immunotherapy.
The neoepitopes identified in this study, including those from tumor-specific mutations, hotspot mutations (for example, KRAS and histone-3 K27M) and fusion proteins, will serve as a valuable public resource for the development of novel therapeutic strategies against childhood cancers.
Comments