Blood cancers are a diverse group of disorders which occur when there is neoplastic proliferation of a malignant blood cell in the haemopoietic system. The clinical presentation of blood cancers is variable and highly dependent on the site and severity of the disease.
Blood cancer classification
Blood cancers are classified into myeloid (related to bone marrow) or lymphoid (related to tissue that produces lymphocytes and antibodies) disorders based on the haemopoietic lineage in which an abnormality occurred; they can also further be categorised into one of the following groups:
Leukaemia is a cancer where malignant haemopoietic cells are found within the bone marrow and peripheral blood. Leukaemia can be classified into myeloid or lymphoid, and acute or chronic based on the rate of onset of the disease. In acute leukaemia, there is abnormal proliferation of blasts (poorly differentiated immature cells) and maturational arrest can occur. In contrast, chronic leukaemia is not associated with blasts, since malignant cells continue to mature during haemopoiesis. There are four main categories of leukaemia: AML (acute myeloid leukaemia), ALL (acute lymphoid leukaemia), CML (chronic myeloid leukaemia) and CLL (chronic lymphoid leukaemia).
Lymphomas affect the lymphoid lineage and are chronic malignancies. Malignant lymphoid cells generally accumulate in, and are restricted to, lymphoid organs causing a lymphomatous static tumour. If the affected lymphoid organ becomes so overwhelmed and accumulated with malignant cells, the cells can force infiltration into organs outside of the lymphoid tissue, such as peripheral blood and bone marrow. Lymphomas are broadly categorized into Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL) based on whether the malignant tumour contains Reed-Sternberg cells (abnormal lymphocytes only associated with HL).
Myelodysplastic syndromes are myeloid malignancies in which immature precursor myeloid cells accumulate in the bone marrow. As a consequence, the death of these immature cells occurs before they can mature into effector cells. This causes ineffective haemopoiesis and consequently a reduction in the red cells, white cells and platelets.
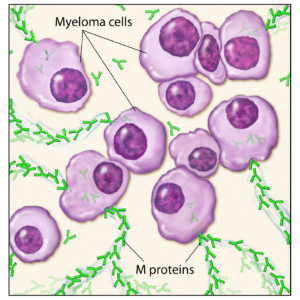
Multiple myeloma is a lymphoid malignancy in which there is abnormal proliferation of malignant plasma cells. In health, plasma cells are required for antibody production; in multiple myeloma, malignant plasma cells over-synthesise and secrete excessive quantities of monoclonal immunoglobulins called paraproteins. In excess concentrations in the plasma, paraproteins can cause severe tissue damage to a number of organs.
Myeloproliferative disorders are myeloid abnormalities in which there is abnormal overproduction of myeloid cells in the bone marrow, most commonly causing erythrocytosis, thrombocytosis, neutrophilia and basophilia. The main myeloproliferative disorders are CML, polycythaemia vera, myelofibrosis and essential thrombocythaemia.
Investigation of blood cancers
The role of a pathology laboratory is fundamental in investigating blood cancer. It is important to accurately diagnose malignancies since treatment strategies vary enormously and failure to correctly diagnose a patient could have a major impact on their prognosis. There are many different tests and analytical techniques that can be employed in the investigation of a suspected blood cancer, including the following:
A full blood count (FBC) provides data on red cell, white cell and platelet indices. These parameters are essential since they detail the number of each cell line and help determine bone marrow involvement. In some cases, the FBC results are one of the first indications of a suspected blood cancer and it can be as a result of FBC analysis that further investigations are requested.

Morphological examination of peripheral blood and/or bone marrow helps identify the shape, size, characteristics, cellular inclusions and maturity of the blood cells. Particular morphological features are distinctly associated with certain types of blood cancer and therefore analysis of morphology is pivotal in aiding a diagnosis or indicating further investigations.
Immunophenotyping analyzes the expression of antigenic markers expressed on cellular surfaces; these markers are called clusters of differentiation (CD) markers. Specific markers associated with each cell lineage allow cellular populations to be identified. In health, certain CD markers should be present, however in malignancy there can be the loss of expression, over-expression and the aberrant expression of specific markers which should not be present in a healthy individual. By comparing results to the normal expected expression, differentiation can be made between healthy cell and malignant cell populations.
Cytogenetics studies cells at the molecular level since some blood cancers are caused by a chromosomal mutation. By analyzing a patient’s karotype and chromosomal structure, genetic mutations can be identified.

Histological examination of a biopsy (for example a lymph node), can reveal tissue architecture including the type of cells present. This helps to determine the presence and/or spread of a malignancy.
Due to the heterogeneous nature of blood cancers, a multidisciplinary laboratory approach is often necessary for diagnosis. Hence, to aid a diagnosis, all laboratory results must be interpreted in conjunction to the clinical presentation.
Innovations and advancements are rapidly progressing in the field of blood cancers with the aim of ultimately helping to reduce the prevalence of such diseases and improve the prognosis for the individuals affected.
Click here to read the latest articles published in Blood Cancer Journal.
Great article especially in the era of potential carcinogens.