
https://respiratory-research.biomedcentral.com/articles/10.1186/s12931-019-1046-6
Respiratory disorders are the second most common reason for children to attend an emergency department. Pneumonia claims the lives of approximately 900,000 children each year, and lower respiratory infections are a leading cause of reduced quality of life and life span worldwide. To help address this, we have developed a tool designed to separate different pediatric respiratory diseases based on the sound of the cough they cause.
We assembled a collaborative research team . . . to develop and test an algorithm that could recognize common childhood respiratory disorders
Accurate and timely diagnosis of respiratory conditions is essential to initiate appropriate treatment. Unfortunately, diagnostic conditions are not ideal in many circumstances which can be due to difficulties with access to trained clinicians or investigations. Doctors need to be physically present to perform a clinical evaluation, which limits the use of telemedicine for respiratory-related consultations. During a time in which telemedicine is globally expanding, we feel it is important to look at new ways of approaching respiratory assessments.
Over the past six years, my research unit has focused on examining the rapid evolution of clinical medicine, particularly the influence of artificial intelligence (AI) in diagnosis. In 2016 I was introduced to Assoc Prof Udantha Abeyratne from the University of Queensland who had conducted exciting work diagnosing childhood pneumonia via analysis of cough sounds in Indonesia. With support from the Bill & Melinda Gates Foundation Grand Challenges in Global Health Exploration grant, he had shown that the sound of a cough carries acoustic information about lower airway pathology.
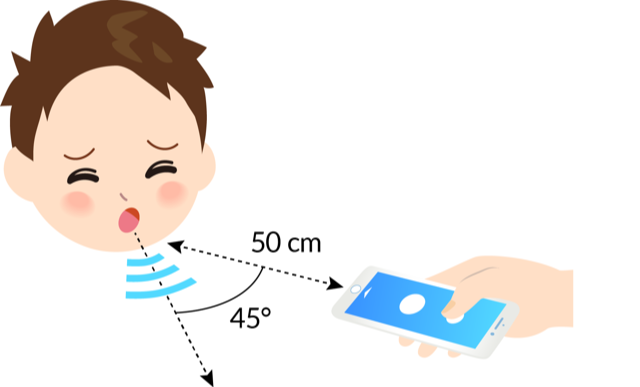
Finding common purpose in improving child health, Udantha and I committed to investigating whether a mathematical algorithm could be trained to recognize characteristics embedded in the cough sounds of different respiratory conditions. We assembled a collaborative research team comprising of pediatric clinicians from Western Australia to collect clinical data and acoustic and AI engineers from Queensland to develp and test an algorithm that could recognize common childhood respiratory disorders. The test would sit on a ubiquitous smart device, such as an iPhone, for easier recording and analysis.
What did we do?
We collected a clinical and cough sound database from 1437 children aged from 29 days to 12 years across two hospitals in Western Australia. From this, we used a training set of 852 patients to develop an algorithm to recognize specific acoustic features characteristic of various respiratory disorders. In our approach, we utilize technology akin to that used successfully in speech recognition: analyzing cough and breath sounds and the associated respiratory sound stream as a ‘language’ with its features operating as phonemes, words and sentences.
We looked at five different conditions: consolidative pneumonia, croup, asthma, bronchiolitis, and the presence of general lower respiratory tract disease (LRTD). We then used the other patients in our database (n=585) to test the accuracy of the tool, compared to clinical panel diagnoses.
What did we find?
The algorithm showed excellent performance in detecting common childhood respiratory disorders. The levels of agreement with clinical consensus were: for asthma (PPA 97%, NPA 91%); pneumonia (PPA 87%, NPA 85%); LRTD (PPA 83%, NPA 82%); croup (PPA 85%, NPA 82%); bronchiolitis (PPA 84%, NPA 81%).
For pneumonia diagnosis, the results exceeded the performance of other scoring systems, including the World Health Organization criteria for pneumonia diagnosis, where tool sensitivity is a priority.
Where can this tool be used?
The advantage that this technology brings is the ability to identify common respiratory disorders without the need for clinical examination, or indeed standard investigations (such as x-rays) or bronchodilator testing. The ability to provide a point-of-care diagnostic output reduces the time between obtaining and waiting for x-ray and other results. For these reasons, the technology would be useful for telehealth consultations and in remote area health services where there is limited access to healthcare.
The tool’s ability to differentiate asthma from pneumonia would be particularly useful in low-income countries where diagnostic guidelines favor pneumonia diagnosis, to the point that up to 50% of children under the age of five years diagnosed with pneumonia could have had their illness reclassified as asthma.
This study shows how new technologies such as machine learning, mathematical modelling and clinical medicine can come together to successfully develop a novel way of assessing and diagnosing disease. We are optimistic that the technology will add to, rather than replace, the stethoscope as a valuable diagnostic aid, to be used when a clinical examination is not possible.
We are now expanding our investigations to look at adult respiratory diseases and to examine the use of our technology to stratify disease severity.
Comments