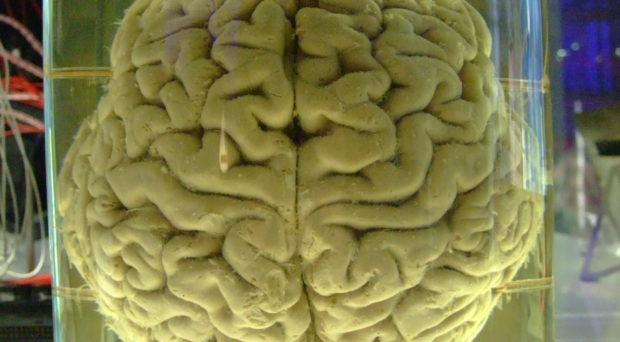
The human brain (Photo credit: Gaetan Lee)
Out of the estimated 438,000 malaria deaths worldwide in 2015, the majority was caused by cerebral malaria (CM). Unfortunately, patients with CM may initially present with the same or similar symptoms as those with uncomplicated malaria. But while patients with uncomplicated malaria usually recover after receiving standard antimalarial treatment, between 10 and 30% of patients with CM die despite treatment.
Is there anything that makes CM unique, that might maybe help health workers to identify patients who are more likely to develop CM than others so that these patients could receive adequate care? Perhaps. CM only occurs in Plasmodium falciparum (Pf), and Pf is the only malaria parasite species that produces histidine rich protein 2 (HRP2). Let’s follow that lead …
The role of HRP2 in cerebral malaria
Already in 1997, a paper reported that HRP2 levels are significantly higher in CM than in uncomplicated malaria. Several recent papers argued that HRP2 levels can be used to distinguish between malarial illnesses and nonmalarial illnesses with coincidental malaria parasitemia (also here, here and here). Moreover, HRP2 levels can predict disease progression as these levels are already significantly higher prior to the manifestation of CM.
Another line of evidence pointing at HRP2 as the culprit for CM starts with the discovery of HRP2 at the Blood Brain Barrier (BBB). In healthy individuals, the BBB protects the brain from harmful substances and organisms. A paper published in 2007 showed that Pf infected red blood cells, which release HRP2 when they burst, weaken the BBB in-vitro.
The latest piece of evidence comes from an in vitro study published in 2016 which found that HRP2 is responsible for the weakening of the BBB.
Quantitative HRP2 testing and adjunctive treatment for CM
Currently there are several Rapid Diagnostic Tests (RDTs) available that show the presence of proteins produced by the malaria parasite. This includes RDTs which detect HRP2.
Quantitative tests do not seem to be available yet; however, an application for the patent of a “histidine rich protein-2 diagnostic test for cerebral malaria” has been submitted. The inventors state that the test will show whether the HRP2 level is low (patient unlikely to progress to CM), medium (patient likely to progress to CM) or high (patient with CM). The test can also be used to identify comatous states caused by nonmalarial illnesses.
The inventors of this quantitative HRP2 test are also part of a research team that observed brain swelling in patients with fatal CM. They concluded that the patients probably had suffered from a compromised brain stem, which hosts the respiratory centre, and that the cause of death was respiratory arrest. Hence, mechanical ventilatory support might have prevented these deaths.
Conclusion
A quantitative HRP2 testing, once fully developed and made available, may become a useful tool for distinguishing between malarial and nonmalarial illnesses and predicting the progression of malarial illnesses. Both types of information are needed for assuring that patients get the right care, and, in doing so, such a test would save many lives.

Comments