Personalized cancer treatment promises more effective treatment and fewer side effects based on a person’s or tumor’s genetic makeup. Next-generation sequencing (NGS) technologies allow large scale genomic testing and data gathering for both clinical and research purposes. However, implementation of complex novel genomics technologies poses major challenges:
- High quality standards are necessary to ensure clinically useful data and to allow data pooling in research databases.
- Harmonized clinical interpretation: What should the scientific standards be for clinical relevance?
- Ethical/legal aspects and societal support: sharing genomic data, expensive treatments, mixed clinical and research use – are all complex issues that may undermine societal trust.
We recently published the Roadbook for the implementation of next-generation sequencing in clinical practice in oncology and hemato-oncology in Belgium. This action plan was required to streamline reimbursement, create collaborative platforms and organize the implementation in clinical care holistically, together with all relevant stakeholders.
Here, we describe the action plan in ten steps. This action plan can serve as a guide for similar initiatives by other countries to facilitate NGS implementation in clinical practice.
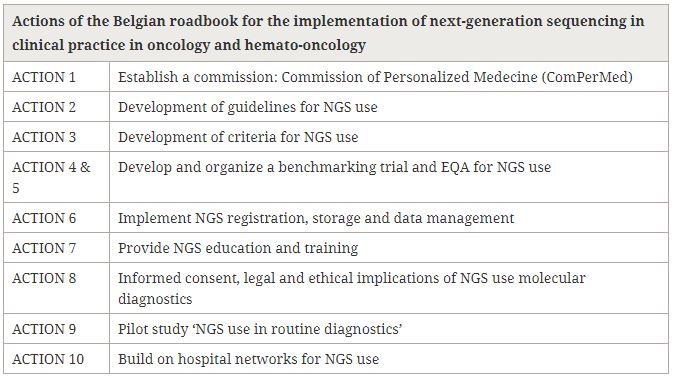
In Belgium, this roadmap is running and resulted in technical guidelines for NGS application in oncology and clinical guidelines describing the genes and regions to be analyzed for specific cancers. Reimbursement of the NGS test is linked to the latter guidelines and to centralized NGS data registration. Several benchmarking studies to evaluate the quality of NGS testing in Belgian laboratories are being performed. NGS education and training is ongoing for pathologists and will be extended to other disciplines. In addition, cancer patients (through focus groups) and citizens (through a citizens forum) are involved in ethical debates and recommendations for policy makers and healthcare professionals will follow soon.
The implementation of NGS testing in cancer is not a uniquely Belgian challenge. The Innovative Partnership for Action Against Cancer (iPAAC) Joint Action brings together 24 partners across Europe. The goal is to develop a roadmap on implementation and sustainability of cancer control actions in different member states, including the use of genomics.
Finally, we want to stress the importance of collaborative processes when implementing genomic technologies in healthcare. On the international level, challenges and successes in different healthcare systems can inform best practices. On the societal level, a thorough debate on the use of genomic data in healthcare can prevent misinformation and distrust. On the national level, good implementation practices will result in efficient investments in better healthcare.
Comments