The United States Dept. of Health and Human Services’ has a goal to reduce MRSA infections by 50%, whose deadline is just under two and a half years away. The data which we have shows that the United States is nowhere near on track for to meet this target. In fact, the most recent data from the National Healthcare Safety Network (NHSN) indicates that our rates may even be increasing, nearing the level of the 2010 to 2011 baseline.
United States Dept. of Health and Human Services’ has a goal to reduce MRSA infections by 50% . . . the data which we have shows that the United States is nowhere near on track for to meet this target.
This finding appeared to not be known by agencies in the U.S. Dept. of Health and Human Services that are responsible for infection control, even though Dr. Kavanagh commented on the uptick in the MRSA infection data at the September 2016 and January 2017 Presidential Advisory Council on Combating Antibiotic-Resistant Bacteria. However, the news media, which is often beguiled by the peer review press, is also hot on the trail of this finding: A testament to the value of the lay press and the need to incorporate their views and findings in the scientific literature.
After contacting our Federal agencies we repeatedly reanalyzed our data. We used two different data files posted late in 2016, and we analyzed the data using the average facility standardized infection ratio (SIR) and the average national patient SIR. All of these analyses produced the same findings. The Centers for Disease Control and Prevention (CDC) analyzed the data a fifth way, using raw non-adjusted data, and found no change between 2014 and 2015.
Questioning the tracking system
This has brought into question using the SIR for the reporting of overall national trends over time. What is evident is that we are currently discussing whether or not MRSA rates have increased in the United States, when the goal was a massive 50% decrease. And that adjustments in the NHSN system may improve interfacility comparisons but this is done at the detriment to the ability to track performance over time.
The reason for the increase found in the NHSN data was attributed to a change in metrics regarding the counting of community MRSA. One needs to ask, what does this have to do with hospital acquired infections? The answer is: Some assert that facilities with high MRSA environmental pressure will also have higher rates of MRSA hospital-acquired infections and, thus, should receive mathematical relief by reducing their MRSA SIR.
The reason for the increase found in the NHSN data was attributed to a change in metrics regarding the counting of community MRSA.
Guidelines for the NHSN stress that even MRSA carriers who are admitted and then develop an infection in a hospital will still be counted as having a hospital acquired infection. But in regions with high MRSA environmental pressure one would expect a large number of carriers being admitted. Doesn’t this adjustment just mathematically negate these reported infections on the back end? In addition, this adjustment mitigates the negative impact of a facility not performing surveillance on admission. Similar adjustments are done based upon bed size and teaching status. If I were to undergo a hip implant, I would like to know the facility’s rate of MRSA, not a down-adjusted value based upon teaching, facility size and environmental pressure.
The United States’ Veterans Health Administration (VA) hospitals have reported over an 80% reduction in MRSA infections. They service a high-risk population and have largely based their control protocols on surveillance and isolation, along with hand hygiene. The United States private healthcare facilities have largely adopted a one size does not fit all system of control with few mandates, which many advocates feel is at risk of degenerating to a ‘do whatever you want’ approach.
The VA and private sector use different tracking systems, with different baselines, to track different types of MRSA infections.
Many, U.S. Institutions, have been implementing universal daily bathing with Chlorhexidine. But how does control of MRSA using these two modalities compare? One cannot answer this question with certainty since the VA and private sector use different tracking systems, with different baselines, to track different types of MRSA infections.
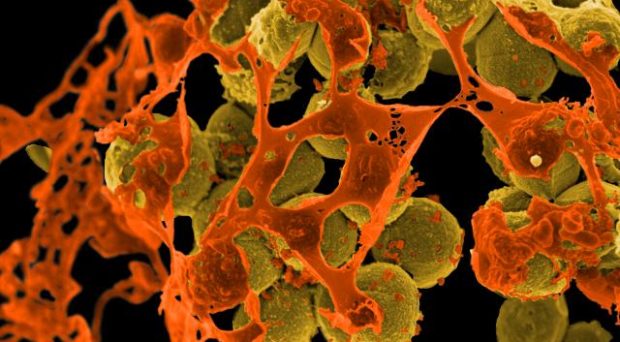
MRSA and other multi-drug resistant organisms need to be recognized for the highly dangerous pathogens that they are. Hand hygiene has become a center point in the United States’ efforts of controlling the spread of MRSA, and I believe this is one of the reasons for our failing to confront this epidemic. If I was a cynic, I would believe this emphasis was an attempt to deflect blame onto staff and avoid the needed investment of additional valuable resources which will be required to reverse this epidemic.
I view hand hygiene for the prevention of MRSA as an important backup measure. If MRSA is being spread by the hands of healthcare workers, then their hands must at one time have become contaminated with MRSA and there must have been a failure of containment and control, which should be viewed as our frontline intervention.
Comments