The horrible crisis that is unfolding in Africa, with ebolavirus infection now threatening to become endemic, has its roots in many causes, of which the current state of understanding of the virus and the means of its control must be the least.
It’s not that we don’t know what to do
Ebolavirus outbreaks can be brought under control within weeks by established containment measures. But in this case, it was three months before the virus was recognized as the cause of the outbreak and another five before WHO declared a public health emergency, with the humanitarian response following only some weeks after that.

Meanwhile densely populated towns, and not just rural areas, are affected; the populations of the affected areas are very mobile; traditional burial practices involve washing the bodies of the dead; and resources for identifying, isolating and treating the infected are very limited. So the outbreak has accelerated, with the number of deaths already exceeding deaths in all earlier outbreaks combined, infections doubling every two to three weeks, and no end in sight.
Accounts from the field, where Médecins sans Frontières has been providing front-line action against the virus since well before it became headline news, make you catch your breath.
Imperatives in the field
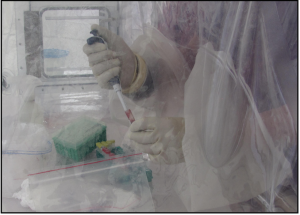
With containment looking like a lost cause at least for the immediate future, the case for accelerated release of unlicensed treatments and vaccines for ebolavirus is a focus of urgent consideration. This month in BMC Biology, Heinz Feldmann, whose research in the Virology Laboratory at the US National Institute of Health (NIH) is on high-containment viruses, and who has field experience with outbreak management, and Thomas Hoenen, also in the Virology Laboratory at the NIH, rehearse the arguments in the context of what we have to hand, what is known about the virus, and the political realities in the field.
None of the existing therapeutic agents or vaccines is licensed. The case for overlooking this for health workers, with priority access to limited supplies, is, as Feldmann and Hoenen point out, more or less incontestable, given the critical importance of trained health workers to all populations affected and the (at least) 144 already lost to the virus.
The case for broader dissemination is more complicated, given that the inherent danger of failure of safety or efficacy will be compounded by the danger of alienating an already terrified and mistrustful population.
Meanwhile, Feldmann and Hoenen are not alone in pointing out that traditional measures for containing the outbreak are imperative, along with simple measures (fluid and electrolyte replacement) for keeping infected patients alive for long enough to give them a chance to fight off the virus for themselves.
Besides, the issue of broader dissemination for experimental measures is for the time being academic. The experimental therapeutic agents and vaccines aren’t available.
It’s not the biology
Everybody knows that after sanitation, the most effective disease control measure is vaccination.
Here’s a very simple fact about vaccines. They depend upon eliciting the natural immune response. If non-fatal infection with a pathogen results in lasting immunity, an effective vaccine can be developed against it.
There are pathogens against which it is very difficult to design a vaccine. Human immunodeficiency virus (HIV) is notoriously one of them, Plasmodium falciparum, the cause of malaria, is another. Failure to develop vaccines against these scourges, despite very considerable effort, is due to properties of the pathogens which mean that we do not develop effective natural immunity to them.
Ebolavirus is not such a pathogen: if we survive, we are immune.
This is not to diminish the difficulties of producing safe and effective vaccines even when this fundamental requirement is met. Live attenuated vaccines may not be completely safe, while subunit vaccines (based on recombinant proteins), which are safe, are not always effective. It takes time to engineer and test a vaccine that combines maximum safety with maximum efficacy – especially if, as in undeveloped countries and emergencies, you need a vaccine that works with just one shot, no boosters.
And because of its very high mortality (estimated for the strain currently ravaging West Africa at 70-90%), ebolavirus requires expensive maximum-containment facilities, so vaccine work has been confined to very few labs which have them.
The two vaccines described by Feldmann and Thoenen in their article are in phase I trials. Their relative merits are still a matter of debate, but there is no dispute about the nine to eighteen months it will take to produce enough doses for mass vaccination.
Here’s another very simple fact (I am not pretending this is news). For purely economic reasons, resources to develop and especially to mass-produce vaccines against very dangerous but rare tropical diseases are extremely limited.
The exposure of 3,000 US troops deployed to contain the virus in Liberia may do something to shift the perceived balance in the cost-benefit equation. The balance will change forever if ebolavirus does become endemic.
Miranda Robertson
Latest posts by Miranda Robertson (see all)
- The scientific Odyssey: Pre-registering the voyage - 3rd May 2017
- A year of almost anything you can think of in life science – an eclectic pick from BMC Biology - 13th January 2017
- Peer review: opting out - 23rd September 2016
Comments