
Multimorbidity – a Twitter investigation
Multimorbidity is the co-occurrence of two or more chronic medical conditions in a patient. Technological and social changes are resulting in increases in both sedentary lifestyles and life expectancy, which in turn lead to more people developing multimorbidity. This trends has begun putting significant pressures on the medical sector and its infrastructure. Nurses, in particular, are faced with significant challenges whilst coordinating multiple care plans for their patients’ individual conditions.

The Florence Nightingale Fodunation took to Twitter to ask nurses four questions related to multimorbidity and encouraged Twitter users to suggest solutions and to debate amongst each other. Twenty-four users responded using the hashtag created by the foundation, #FutNur, potentially reaching over 50,000 Twitter users. In a recent paper, O’Connor et al. used these data to research what nurses believe is needed to care for patients with multimorbidity.
The replies were grouped into five particular themes of what the nursing profession must focus on in order to effectively cope with morbidity. Helping patients and their friends and family deal with the burden of having multiple chronic conditions was the initial focus. Next was the type of care nurses need to deliver, with the respondents believing holistic care is essential. Additional themes were the need for more evidence on methods of treating multimorbidity and the quality of education nurses receive regarding this issue. Finally, the respondents expressed a frustration in the way the health services were designed, and several suggestions were made to improve it.
The authors concluded that Twitter, and other social media, can potentially be very helpful in research amongst health professionals. Furthermore, they found that there are many ways in which coping with multimorbidity can be made easier. These include investing in research and nursing education surrounding the topic and creating better tools and guidelines to help nurses care for those with multimorbidity.
From apprehension to advocacy: nursing students’ experiences with care home placement
As populations around the world age, more nurses with experience caring for older adults are needed. However, lack of interest among nursing students and insufficient education in nursing schools focused on care of older adults have contributed to a nursing workforce, already stretched thin across all fields, that is not prepared to care for this growing demographic. One potential solution is placement of nursing students within residential aged care (RAC) settings for clinical education.
In order to explore key stakeholders’ experiences with nursing student placement in RAC, Moquin et al. conducted a qualitative study using a participatory action research approach. Nursing students were interviewed both before and after placement, and their instructors, RAC staff, and residents were interviewed after.
The study found that although students began their placements with a range of concerns, over the course of the placement, they became comfortable in the setting and actively engaged with and advocated for the residents. Although many of the students indicated that they were unlikely to pursue a career in RAC, they did value the skills learned and felt that they would be better prepared to care for older patients in other settings.
Nurses’ experiences of an unfamiliar method of assisted suicide
Assisted suicide in Switzerland is legal and not uncommon. Voluntary Stopping of Eating and Drinking (VSED) is a method of actively hastening one’s own death, and doesn’t require a doctor’s approval or a terminal diagnosis, though it does often require medical support from nurses or medical staff. It is the individual’s choice, and it allows them, and their friends and families, time to prepare for their death. But how do nurses feel about VSED in their professional role?
Saladin et al. conducted an embedded single case study of a patient living in a long-term care institution choosing to end her life via VSED. By conducting group and individual interviews, they gathered information regarding the impact of this choice on those closest to the patient, including relatives and care institution staff.
The results of the interviews showed that the nursing staff felt obliged to help the patient hasten her death via VSED, as it was her choice to do so. They further described how the general manager of the institution initially did not want to allow VSED to occur, but the nursing staff advocated for the patient. In doing so, the staff sometimes struggled between caring for the person and arguing with the institution they worked for. They had to find an acceptable way both for the patient to be allowed to choose her death and for the institution to be comfortable with the process.
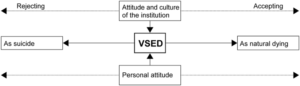
The study concludes that the attitude of the institution itself can be decisive in how VSED is dealt with; VSED can be perceived as suicide or as natural dying, and institutions are generally less comfortable with the former. Therefore, the authors believe it is important that health care professionals develop a professional opinion of VSED, thereby benefiting patients who choose VSED towards the end of their lives, as well as their relatives and those who care for them.
Nursing education challenges and solutions in Sub-Saharan Africa
Many of the healthcare interventions launched as part of the Sustainable Development Goals rely on a sufficient workforce of nurses with relevant competencies, but Sub-Saharan Africa has an estimated shortfall of 600,000 nurses needed for these initiatives. Improvements in nursing education are needed to increase the nursing workforce and improve the quality of healthcare. This review from Bvumbwe and Mtshali integrated literature reporting on nursing education challenges and their solutions, in order to identify needs for and possible methods of improvement.
Systematic and targeted searches of academic and gray literature led to a final sample of 20 academic and five gray-literature articles. Thematic analysis was used to identify six themes, representing different challenges and their possible solutions: curriculum reforms, professional regulation, transformative teaching strategies, collaboration and partnership, capacity building, and infrastructure and resources. Within each of these areas, gaps and unmet demands were identified along with reforms and interventions that were beginning to address them in some contexts.
This review highlighted common challenges in nursing education faced by many of the countries in Sub-Saharan Africa, from lack of infrastructure to insufficient faculty. Strategies to address these challenges are being implemented and this review points to those that have had positive effects and to where further efforts are needed.
Comments