Cancer of the pancreas continues to be an active area of research. It is a common cancer all over the world and continues to be one of the most lethal. About 99% of patients with cancer of the pancreas have adenocarcinoma, a type of malignant tumor, and the 5-year survival rate for patients with adenocarcinoma of the pancreas is about 3-5%.
The survival rate has improved somewhat in recent years because of developments in surgery and surgical critical care, resulting in better results after resection. However, despite aggressive surgical resection, 95-97% of these patients still die within 5 years. One of the problems is that there are no adjuvant treatments (therapy applied after surgery) which are routinely effective. Surgery is most effective in patients with early stage disease but approximately 90% of patients with the disease already have metastases at the time of diagnosis and surgery will not benefit them.
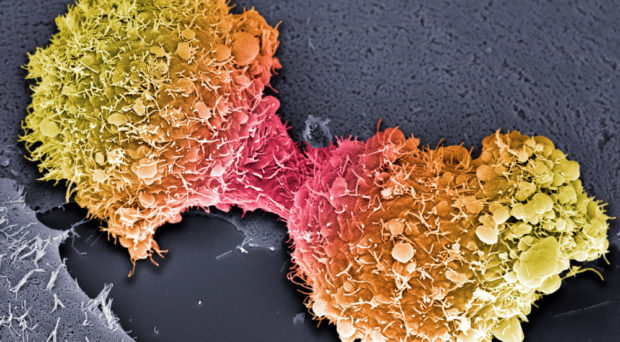
There are many investigators studying the characteristics and growth of pancreatic cancer at the cellular and sub-cellular levels. This approach may eventually result in the development of effective therapies, although this may take a long time. It is hoped, for example that immunotherapies could be developed to attack specific, but as yet unidentified, markers on the cell surface of pancreas cancer cells. Understanding malignancies at the cellular and sub-cellular level is essential for the development of effective therapies.
Complementing cellular research with computer models
The computer models we are developing may assist in identifying the best time to administer a yet to be developed agent that is effective against pancreas cancer.
Another approach is the one we are taking, to study the growth of the entire tumor in the patient, using data from computed tomography imaging. We are obtaining this data and fitting it to innovative models of cancer growth. This approach is complementary to cellular research to develop an effective adjuvant therapy for this disease.
The computer models we are developing may assist in identifying the best time to administer a yet to be developed agent that is effective against pancreas cancer. Our expectation is that we can use a computer model to understand the growth of the entire tumor based on data from other patients. Ultimately this approach may contribute to the effectiveness of future agents against pancreatic cancer.
The approach we are taking to treating pancreatic cancer should also help to improve awareness and understanding of this disease. We are using computer models, which is a new approach to cancer therapy. One aspect of this approach is that people will be able to understand exactly where their own tumors fit into the pattern of data from many other patients. This results in a form of “personalized therapy” where the timing of administration of the anticancer agent would depend on the growth pattern of the patient’s individual tumor growth pattern.
There is little question that the current outlook for therapy given to patients with cancer of the pancreas is bleak. The only curative treatment is surgery but only 10% of patients with the disease are even eligible for surgery. We must continue to develop new approaches to therapy. The research we are doing may help to guide optimal administration of these new treatments, with a personalized approach based on the growth characteristics of a patient’s own unique tumor.
Comments