Numerous sophisticated laboratory and computational methods have been developed to identify the sheer complexity of the composition of microbial communities, as well as the molecular interactions among microbes and with their host. The recent logarithmic increase in the number of scientific papers and books, referring to the human microbiota in health and disease, reflects the great impact caused by this topic on biology in general as well as medicine in particular.
The complex and prolific laboratory output from microbiome science is barely assimilated into common clinical practice.
As opposed to traditional microbiology, widely adopted by physicians, the complex and prolific laboratory output from microbiome science is barely assimilated into common clinical practice. Here, we take a quick look at the long-term success in the implementing laboratory methods used by traditional clinical microbiology for the diagnosis of infectious diseases, and comment on the extraordinary delay in the adoption of microbiome data into the mainstream of clinical practice.
Traditional clinical microbiology
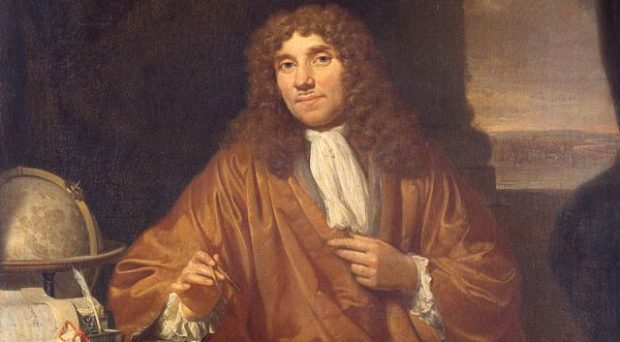
To our knowledge, the first observation of bacteria under the microscope was done and documented by Antonie van Leeuwenhoek in the late 17th century. Gerhard Henrik Armauer Hansen in 1873 was the first to see under the microscope a human pathogen- Mycobacterium leprae, which ironically enough still resists culturing in artificial media. Nowadays, microscopy is frequently used to detect microbes in clinical specimens, including body fluids and tissues.
Culturing microbes in vitro is a powerful method which allows a multi-faceted characterization of their taxonomy, metabolism, virulence factors, in-vitro susceptibility to antimicrobials and fingerprinting for epidemiologic investigations.
More recently, a broad collection of molecular methods enabled the detection and characterization of microbes, those involved in a specific infection and also the ones colonizing a specific area and occasionally threatening the host. These tests can be directed to detect specific sequences of DNA or RNA, identify metabolites or their combinations, which can robustly identify specific microbes.
Current reporting of microbiome data
Microbiome data allows the study of the composition of microbial communities, in both healthy people and patients with metabolic and inflammatory diseases. Molecular methods are used to establish the microbial composition of a sample, by sequencing the microbiome of a particular site.
Shotgun metagenomics and 16S rRNA sequencing are culture independent techniques commonly used to investigate microbial communities. However, these procedures are very difficult to interpret by practicing physicians. There are two main reasons for this: the multi-dimensional complexity of ecologic communities and the spectral and dynamic conformation of these values.
Making microbiome data digestible to practicing physicians
To facilitate the adoption of microbiome data by physicians, we suggest adapting and importing analytical methods used in economics, to overcome complex, dynamic and interconnected sets of data. Instead of using intricate multidimensional graphics or formulae, the idea is to employ simple arithmetic or geometric scales to summarize the data regarding a given microbial community.
Minimizing the number of parameters will open the door for the appropriate inclusion of microbiome data into the clinic.
Machine learning algorithms have been recently reported to gather and analyze satellite data including nightlight intensity and other daytime landscape parameters to define degrees of poverty. Microbiome science may benefit from these models which significantly simplify very complex data sets. Assessing normality, predicting imminent crises and evaluating fluctuations as indicators of recovery, are major goals when harnessing human microbiome data of various body sites. Minimizing the number of parameters will open the door for the appropriate inclusion of microbiome data into the clinic.
In the article collection ‘Clinical insights into the human microbiome’ published in BMC Medicine, we explore the most recent and exciting findings on how the microbiome shapes physiological responses and affects treatment. Examples of featured topics include the gut brain axis, the role of microbiome in treatment outcomes, immune response and microbiome diversity and the effect of antibiotics in children. Don’t forget to read the articles here, and if you have any presubmission queries about the collection, please email us at bmcmedicineeditorial@biomedcentral.com
Comments