
What is a traumatic pneumothorax?
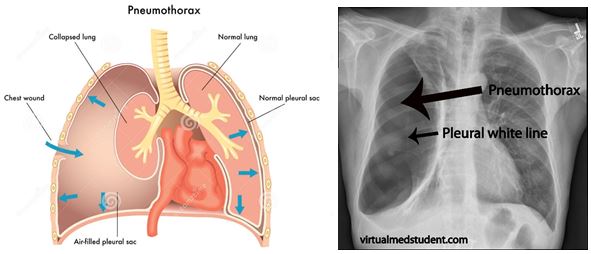
A traumatic pneumothorax is an injury to the thorax caused by motor vehicle accidents (MVAs), falls or/and wounds, and can be present in penetrating or non-penetrating trauma to the thorax. It can be life-threatening and requires emergency management.
It results from air entering the potential space between the two membranes surrounding the lung – the visceral and parietal pleura, leading to a progressive collapse of the lung and subsequent impairment of the respiratory function. The ultimate risk is the creation of a tension pneumothorax leading to cardiac arrest if not immediately needle decompressed.
How to solve it?
Once diagnosed, a traumatic pneumothorax most of the time requires drainage. In some cases observation and aspiration of an asymptomatic pneumothorax may be appropriate, but the choice should be made by a qualified physician.
The recommended technique for pneumothorax drainage is the surgical procedure, which has less risk of injury to the thoracic vessels or heart than the blind insertion of a chest tube with a trocar. The surgical approach implies a dissection of the chest wall, which is well known from surgeons but not so from emergency physicians (EPs) who are not used to it, whereas they may see most of traumatic pneumothoraxes on the front line.
Consequently it can be very stressful for an EP to perform a surgical chest tube insertion to drain a traumatic pneumothorax, with the risk of errors or failure. Furthermore, a traumatic pneumothorax represents a low-volume, high-stakes situation exposure per EP, which makes it more stressful.
Approaching this learning need
If clinical experience under supervision cannot provide sufficient input to learn a procedure, simulation can be an alternative learning style. Because Advanced Trauma Life Support (ATLS) courses were not spread enough in France, we found out that there was a real need for teaching emergency residents (PGYs) and EPs from our area (1.8 million, level-3 university hospital) how to surgically insert a chest tube in case of a traumatic pneumothorax. Therefore we set out a specific simulation program within a University course to learn how to surgically insert a chest tube.
How did we do this?
Simulation-based training requires a model and an evaluation tool. Because we did not find any convenient simulation task-trainer for the surgical approach to be sufficiently realistic (it was our primary objective), we decided to look for an animal model.
After several tries we chose the lamb chest wall and constructed a new task-trainer using a lamb chest wall fixed on a plastic box with a webcam feedback to see the endothoracic steps of the procedure (photos). Use of this model can be viewed in our video below:
The surgical approach is very precise and unfortunately there was no published evaluation tool detailing the different specific steps of this procedure. Therefore we designed and validated a performance assessment scale for chest tube insertion in case of traumatic pneumothorax. This scale has a good validity (Cronbach alpha = 0.747) and a very high reliability (intra-class coefficient = 0.966).
What were our key findings?
We randomized 65 PGYs and EPs to a specific simulation-based training in surgical chest tube insertion on our model with our performance assessment scale. Success rate and performance score of the group who underwent simulation training were significantly higher than those who didn’t (respectively 97% (SIM+) vs. 58% (SIM-), and 16.29±1.82 (SIM+) vs. 11.39±3.67 (SIM-), both p<0.001).
Surprisingly there was no difference between the SIM+ and SIM− groups regarding status (p=0.44) or previous surgical insertion (p=0.12). This was related to the rare exposition to the clinical situation and to the absence of regular spread ATLS courses in France.
In conclusion simulation-based education significantly improved the success rate and performance of surgical chest tube insertion on a traumatic pneumothorax model in our population of emergency residents and physicians. Therefore, such a program could be initiated if a possible gap in performance in surgical approach is detected.
Comments