Researchers have reported today in Breast Cancer Research that women with breast cancer who take anti-oestrogen treatments for longer could reduce their risk of developing the disease in the opposite breast.
The drugs in question are those used to treat hormone-positive breast cancer, the most common form of the disease which accounts for around 40,000 of the 50,000 cases diagnosed each year in the UK.
Today’s results might sound familiar. That’s because we’ve learnt from a procession of landmark trials in recent years that women who take anti-oestrogen treatments for ten years rather than five are less likely to see their breast cancer return, and in some studies were more likely to survive the disease.
Not surprisingly then, these results have been practice changing. Official breast cancer treatment guidelines in the US and Scotland now recommend that women take anti-oestrogen drugs for ten years rather than five, and while NICE guidelines for England and Wales are yet to be updated many clinicians are already recommending extended treatment.
With around 11,500 women still dying from breast cancer every year in the UK it’s crucial that we find new treatments for the disease, but also that we find out how to use the drugs we already have to save as many lives as possible. So why is it that for many women living with the disease, results like today’s aren’t always a cause for celebration?
Struggling with the side effects
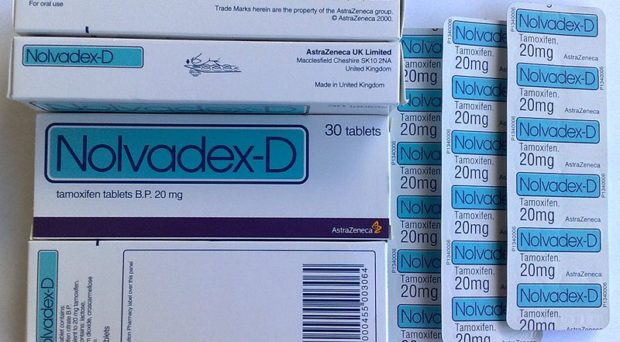
It’s thought that around 40% of women taking the anti-oestrogen drug tamoxifen experience hot flushes and sweats
It’s an unusual week at Breast Cancer Now if we haven’t heard from women who are struggling with the side effects of their treatments. It’s thought that around 40% of women taking the anti-oestrogen drug tamoxifen experience hot flushes and sweats, 25% experience fatigue and 10% experience discharge from the vagina, dryness or itching.
For some, their side effects can be disruptive and unpleasant, but on the whole bearable. For others it’s an entirely different story, and the pain and discomfort are so severe that they feel they have no choice but to stop treatment. But just how common is this?
Funded by Breast Cancer Now to answer this question, scientists revealed in 2013 that more than half of women with breast cancer weren’t taking their anti-oestrogen medication for the full five years.
During the first year of treatment women collected, on average, 90% of their tablets. Over the next three years this figure dropped to 82%, 77% and 59% respectively. By year five half of the women were collecting 51% or less of their prescription.
Most worryingly though, this increased women’s chances of their cancer returning and their risk of dying. In a follow up study, the team calculated that more than 400 lives and £30 million a year could be saved if patients were better supported to take their tamoxifen for the full five years they were being prescribed.
Providing support
It was clear that we needed to take action, so Breast Cancer Now commissioned a study which is now underway to improve the availability of cognitive behavioural therapy
These are staggering figures, before even taking into consideration the lives that could be saved with an additional five years of treatment. It was clear that we needed to take action, so Breast Cancer Now commissioned a study which is now underway to improve the availability of cognitive behavioural therapy which has been shown to be effective at minimizing the impact of hot flushes and night sweats.
We’re also funding a team of health psychologists at Kings College London to understand why women stop taking tamoxifen, and develop new ways to support them. The side effects of anti-oestrogen drugs can be harsh, but we know this isn’t the only reason people stop taking them.
Sometimes patients aren’t fully aware of the importance of taking the entire course as prescribed, or they simply forget. By speaking to patients and understanding all of these factors our scientists will be able to help them get the most from their treatment.
A complicated problem
What’s clear is that patients, healthcare professionals, scientists and charities need to work together to find solutions to this complicated problem. And that’s why initiatives like the National Cancer Research Institute (NCRI) Breast Clinical Studies Group Working Party on Symptom Management are so important.
This is a group of expert patients, researchers and charity partners – including Breast Cancer Now – who have come together to carry out research and campaign for better evidence-based treatment guidelines for dealing with the side effects of breast cancer treatments.
At Breast Cancer Now we have a big ambition, that by 2050 no woman should die from breast cancer. And while it’s undoubtedly good news that extending treatments could save hundreds if not thousands of lives in the long term, our vision for the future is one where women with the disease can live their lives to the full. It’s only by understanding the experiences of those living with the disease right now and what matters to them that we’ll find the treatments and support they so desperately need.
Interestingly, my wife suffered badly with side-effects from the first brand of Tamoxifen. She was changed to that of a different manufacturer (Wockhardt) and was fine. Possibly coincidental.