
The first thought one has of San Francisco is the beautiful Golden Gate Bridge, described as “possibly the most beautiful, certainly the most photographed, bridge in the world”.
San Francisco also brings to mind a hub of technology and innovation, being home to many industry leaders and universities. It was therefore fitting that it was the setting for this year’s Consortium of Universities for Global Health (CUGH) conference, whose theme was ‘Bridging to a sustainable future in global health’.
This is particularly timely after the recent transition from the Millennium Development Goals to the Sustainable Development goals, and relevant due to the current Zika crisis and the unfinished agenda of global health inequities, such as nutrition and smoking.
Planetary Health
Of increasing importance to global health is the issue of planetary health- the idea that the health of humans is dependent on the surrounding environment, and that any measures to protect and improve human health should also take into account the health of the planet.
In a panel session, Samuel S. Myers gave an excellent presentation on the complex nature of planetary health, discussing the current ecological paradox that we are facing.
This paradox is the relative success that we are enjoying in terms of public health despite the simultaneous occurrence of ecological degradation. The paradox can be explained by the current generation mortgaging the health of future generations for present benefit – a situation that is unsustainable.
But how can we resolve this situation? The panel made a strong argument for a more cohesive trans-disciplinary nature of planetary health that would be an alliance of research, education and policy.
Collaboration in global health technology

The need for better collaboration among different fields was a central argument of the conference.
In a packed session on global health technology, panelists who were experts in bioengineering, mHealth, big data and precision medicine discussed their experiences in what they considered to be game changers in this fast-moving field, especially in resource-limited settings.
Carlos Bustamante gave a stand-out presentation about the challenges and opportunities in personal genome information, discussing the Precision Medicine Initiative launched in 2015, and the ways in which this could be used to generate new drugs and targets, as well as better understanding genetic predisposition to disease.
He cautioned that participants, whose data is used in these initiatives, should be as diverse as possible, in terms of ethnicity and socioeconomic status, or else there is the possibility that new technologies will increase the risk of health inequities due to under-representation from certain sectors of society.
Of course, concerns were raised regarding affordability and sustainability of these technologies.
For instance, many low- and middle-income countries (LMICs) are provided with equipment from higher income countries in order to meet health needs. However, lack of maintenance and reagents will often render these technologies useless after a short period of time.
The panel highlighted that there should be more opportunity for LMICs to innovate these technologies themselves so that they will be better able to maintain them. This requires a collaborative effort among health workers and engineers to motivate the foundation of innovation hubs in LMICs.
Interconnectivity: a risk for global health security?
Planetary health also underscores the importance of our interconnected world, with the real risk of global pandemics and the issues that can arise if the ecological balance is upset.
The current Zika crisis, and recent Ebola crisis, perhaps demonstrate the vulnerability of global health as a consequence of interconnectivity.
A few sessions in the conference addressed these issues. Jason Cone from Médecins Sans Frontières (MSF) gave an overview of holes in global health security leading to susceptibility to pandemics.
He highlighted that LMICs are particularly vulnerable to pandemics due to lack of adequate public health infrastructure, and also lack of innovation in research and development.
Innovations that might prevent or suppress a pandemic are often inaccessible to LMICs, for instance, due to high price models of that innovative technology or intervention. He highlighted that disease outbreaks only tend to precipitate change when they become pandemic and threaten high income countries.
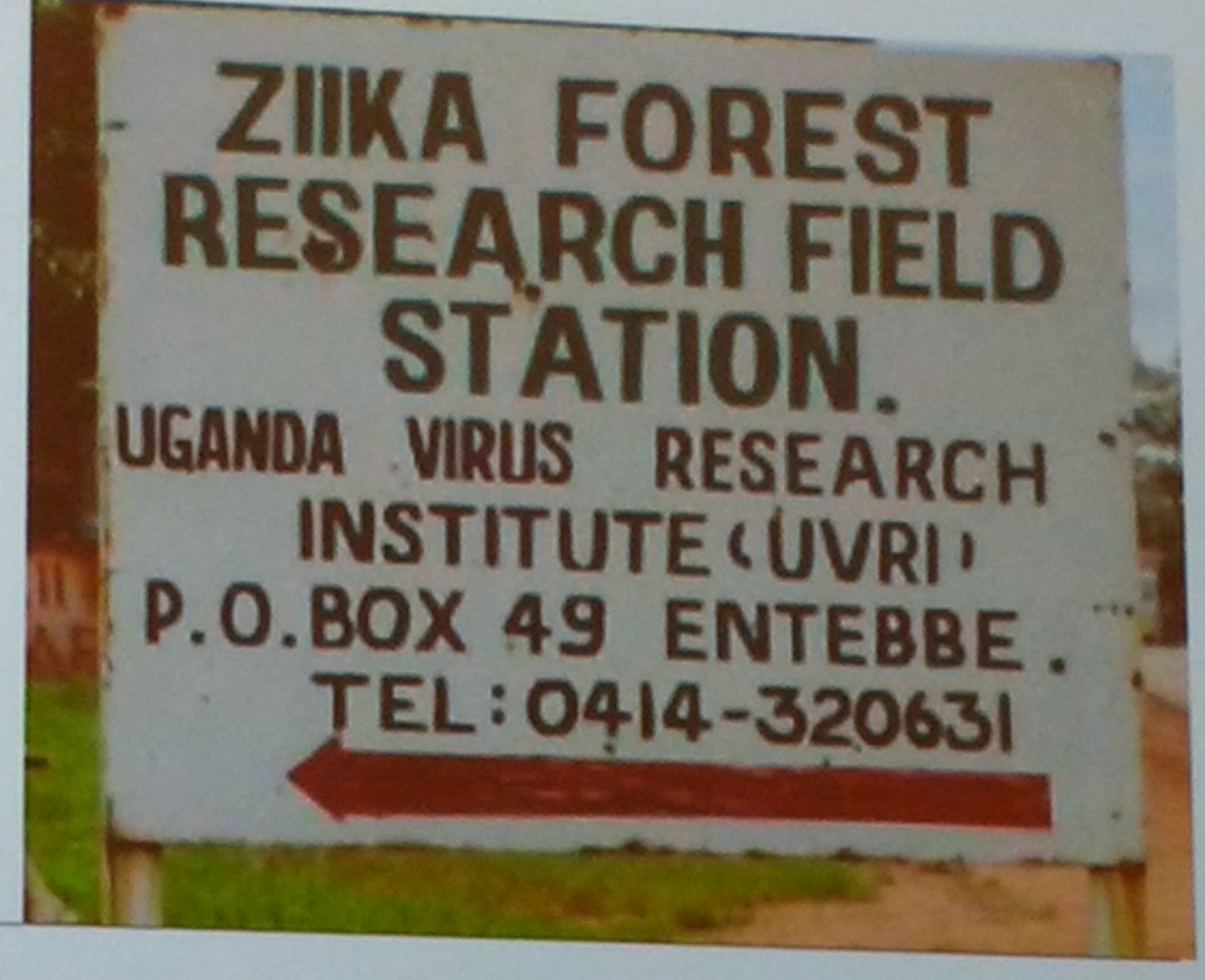
One such example is Zika virus, which is associated with fetal abnormalities in pregnant women who have been infected.
Jonathan Patz made a strong case for Zika outbreaks being linked with preceding dengue outbreaks and high temperatures due to El Niño, which makes a strong case for planetary health.
Diagnosis of Zika infection remains a problem; Patrick Kachur gave an overview of the challenges in diagnosis due to issues regarding cross-reactivity.
Uncertainties also remain regarding the consequences of Zika infection other than microcephaly. Kathy Spong and Eva Harris discussed their work on forthcoming longitudinal cohorts to establish other potential complications of the disease.
In these fast moving fields, it will be interesting to see if new technologies and better collaboration can aide in increasing global health security and improved planetary health. Overall, the conference stimulated debate in these areas, pushing for innovative strategies to deal with these and forthcoming health challenges.
BMC Medicine will be launching a new article collection in late 2016, Medicines and the Future of Health, in collaboration with the Journal of Pharmaceutical Policy and Practice (JoPPP). This collection will cover recent advances in drug and diagnostics development, precision medicine, medicines use, policy and access, which have both broad interest and high clinical and public health relevance due to their impact on the future of health.
If you have any research you would like us to consider for inclusion in our Medicines and the Future of Health collection, please email the journal at bmcmedicineeditorial@biomedcentral.com.
 BMC Medicine: passionate about quality, transparency and clinical impact
BMC Medicine: passionate about quality, transparency and clinical impact
2015 median turnover times: initial decision three days; decision after peer review 40 days
Comments