Multiple sclerosis (MS) is the most common disabling neurological condition affecting young adults, with around 2.5 million cases worldwide, and around 6,000 new diagnoses in the UK every year. It’s an inflammatory demyelinating condition of the central nervous system (CNS) that’s characterized by the destruction of myelin – a fatty substance insulating nerve fibers – resulting in the formation of scars (known as lesions or plaques) which disrupt the transmission of impulses.
The heart of the matter
One of the most important aspects of the fight against multiple sclerosis is the conducting of clinical trials. Luigi Grimaldi, the Editor in Chief of the newly launched BioMed Central journal Multiple Sclerosis and Demyelinating Disorders is at the forefront of MS research, heading up a multiple sclerosis clinic at the Fondazione Istituto San Raffaele “G Giglio” of Cefalù (Italy) which is involved in a range of pharmaceutical clinical trials.
We are still consistently far behind a ‘cure’ for MS and even today’s effective treatments have a consistent quota of patients that simply do not respond to them
Luigi M E Grimaldi
Editor-in-Chief, Multiple Sclerosis and Demyelinating Disorders
Following the new journal launch, I asked him why he feels clinical trials in MS research are so important. He highlighted the immense commitment from global pharmaceutical companies and the scientific community in the development of new treatments.
He also told me that “we are still consistently far behind a ‘cure’ for MS and even today’s effective treatments have a consistent quota of patients that simply do not respond to them”, which really illustrates the importance of developing new and innovative treatments so that all sufferers can benefit from treatment.
Putting the brakes on disease progression
Last year saw big changes in the treatment of people with the most common form of MS, relapsing-remitting MS (RRMS). In the UK a new consensus has been reached, recommending that these patients receive treatment with a disease modifying drug closer to the time of diagnosis and for the effectiveness of the drugs to be more closely monitored.
Despite the range of available drugs currently recommended for the treatment of RRMS, investigators are constantly trying to find better and more effective treatments to stop the progression of the disease. For example, a study taking place in Cambridge is looking at whether treatment using the anti-cancer drug bexarotene is able to promote remyelination in people suffering from RRMS. This work is incredibly exciting for people suffering from RRMS, and in time could lead to revolutionary new treatments becoming widely available.
But what’s new for those suffering from the elusive, progressive forms of MS? Progressive MS – both primary and secondary – is a particularly ‘hot topic’ in MS related research at the moment. Currently, none of the drugs used to treat RRMS are used in the treatment of people with primary or secondary progressive MS, and so research in this area is particularly important.
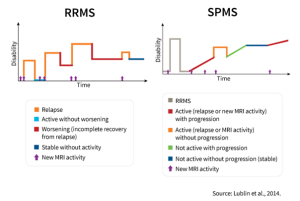 Around 85% of MS sufferers are diagnosed with the relapsing remitting type. This is where the sufferer has sudden flare-ups of symptoms (relapses) followed by periods where the symptoms are very mild or disappear completely.
Around 85% of MS sufferers are diagnosed with the relapsing remitting type. This is where the sufferer has sudden flare-ups of symptoms (relapses) followed by periods where the symptoms are very mild or disappear completely.
Many patients diagnosed with RRMS will eventually develop the secondary progressive form (SPMS), which typically emerges 10-15 years after disease onset.
This form is characterized by a slow, cumulative worsening of disability, rather than relapses followed by recovery. This is shown in the image above.
The MS-SMART study is a ground-breaking new UK study which is investigating whether any of three drugs – fluoxetine, riluzole and amiloride – could help to slow the rate of brain volume loss in SPMS and therefore slow or stop worsening of disability.
This large-scale, UK based study is definitely an important step in the right direction when it comes to putting the focus on novel treatments for SPMS.
Researchers are by no means short of ideas in this area. For example, the recently completed CUPID study looked whether the active ingredient in cannabis, tetrahydrocannabinol, could help to slow the course of progressive MS. Another example is the ACTiMuS study, recently published in Trials, which examines the neuroprotective and reparative potential of bone marrow derived stem cells in the treatment of progressive forms of MS.
Only part of the problem
Despite all of the excitement surrounding disease modifying drugs, it is important not to forget the treatments for the everyday symptoms of MS.
Fatigue is one of the most common symptoms, reportedly affecting around 80% of sufferers; this means that research into this area has really taken off. For instance the ELEVIDA study, currently underway in Germany, is looking at the effectiveness of a web-based psychotherapy program in the treatment of fatigue.
Another study published in Trials connected to three linked records in ISRCTN compares the effectiveness of three different rehabilitation strategies in treating MS-rated fatigue: aerobic training, cognitive behavioural therapy, and energy conservation management.
Fatigue is one of the most common symptoms, reportedly affecting around 80% of sufferers
The decline in cognitive function (thinking, memory and attention) is another symptom that is reported by many MS sufferers, and so is drawing attention in research. For example, the CRAMMS study investigates the effectiveness of cognitive rehabilitation for improving memory and attention in people with MS.
Taking a step forward
For MS sufferers, the single most important thing is – unsurprisingly – to improve quality of life. I recently spoke to Serriye, who was diagnosed with RRMS in January 2002. She told me that “when you have MS you want to work with what you have, and exercise is a good place to start”.
She also showed interest in the idea of combining physical therapy and psychological training. She told me that “the mental barriers you put up stop you from doing the exercise you want to do that could improve your life.”
When you have MS you want to work with what you have, and exercise is a good place to start
Serriye
MS patient
When asked about her opinions relating to current research, Serriye felt that more information about the current research should be “put out there for people” with the condition, as it’s difficult to know what’s really available.
Luigi Grimaldi also has some interesting views on physical rehabilitation trials in the field. He acknowledges that this field is still in its infancy when it comes to designing effective clinical trials that are not restricted to whether the patients experience improvement, but through appropriate endpoints which will “complete the therapeutic armamentarium of the caring clinicians.”
There is no shortage of new trials looking at physical rehabilitation for MS patients. For example, the Sheffield ExIMS trial looks at whether a 12 week exercise program is an effective means of improving mobility and functioning in patients with mild to moderate MS. On the other end of the spectrum, the SUMS study looks at the clinical and cost effectiveness of a home-based standing intervention, using a specialized standing frame to help severely disabled people with progressive forms of MS.
In recent years, advances in technology are having more and more impact on rehabilitation practices
In recent years, advances in technology are having more and more impact on rehabilitation practices. For instance this pilot study, recently published in the Journal of NeuroEngineering and Rehabilitation, looks at the effectiveness of the CAREN (Computer Assisted Rehabilitation Environment) virtual reality system in improving balance in MS patients.
The future’s bright
Most people know someone affected by MS, either directly or indirectly. The simple truth is that there is currently no cure, but through the continuous efforts of the scientific community, that may not be the case for much longer.
Whether through the development of novel medications or the repurposing of existing ones, creating innovative treatment options for debilitating symptoms or improving physical rehabilitation, things are looking up for MS sufferers around the world.
Comments