
Researchers already know how to theoretically cure a significant proportion of all human cancers. The problem is actually doing it.
At the heart of this challenge lies a molecule called MYC. In the same way that a conductor directs all the various parts of an orchestra to work together in harmony, MYC co-ordinates the actions of many different genes inside cells to keep things running smoothly.
From controlling cell division and growth, to instructing faulty cells to die, MYC has been linked to a wide range of fundamental biological processes – something we’ve written about in depth in this post. And, unsurprisingly for such a ‘super-controller’, faults in MYC have been linked to many different types of cancer.
Researchers have long known that faulty, overactive versions of MYC can lead to cells dividing out of control – like a conductor whipping an orchestra into a chaotic, frenzied crescendo – ultimately leading to cancer.
In fact, overactive MYC is found in up to seven in ten tumors of all kinds, from aggressive lung cancers to childhood brain tumors. As a consequence, researchers around the world have focused a huge amount of effort on trying to switch it off.
Unfortunately, switching off MYC is turning out to be an enormously complex puzzle. And that’s why we’ve set the challenge of solving it.
Switching MYC
Although researchers have known about MYC since the 1980s, the fact that it does so many different things inside cells means it’s tended to be overlooked as a target for cancer drugs.
Surely, the argument goes, it’s impossible to hit MYC, and stop cancer cells dividing, without also messing up all the other vital processes it’s involved in?
But in the past five years or so, a team of Cancer Research UK-funded researchers in Cambridge have proved everyone wrong.
Using genetic engineering techniques, they’ve created mice whose MYC gene could be specifically switched off throughout their whole bodies. When these animals developed lung cancer, turning off MYC completely killed the cancer cells.
Importantly, the treatment only caused mild, reversible side effects, suggesting the impact of temporarily blocking MYC in the rest of the body – which is what would happen with a drug – might not be as severe as was first thought.
These remarkable results re-ignited interest in targeting MYC as a potential cancer cure. But the system that Cambridge team used relies on complex genetic engineering – something that’s not technically or ethically possible in humans – and the hunt is on to find drugs that can stop MYC in its tracks.
But it’s not a simple task, as our chief scientist, Professor Nic Jones, tells us: “All the evidence would suggest that MYC is a good target, and there have been efforts to develop drugs to block it. But so far those efforts have failed, and it’s going to take a completely different way of thinking to achieve it.”
Understanding the reasons for this failure explains why targeting MYC is such a Grand Challenge.

Drugging the undruggable
The targets of most ‘smart’ drugs, such as trastuzumab (Herceptin) or vemurafenib (Zelboraf), are usually signalling molecules found on or inside cancer cells. These tend to have a very well-defined shape and structure, with neat biological ‘pockets’ that drugs can be slotted into, like a key fitting into a lock.
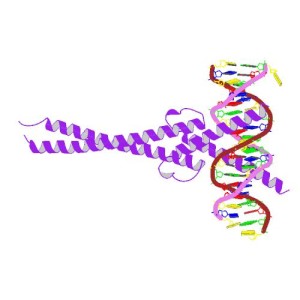
MYC is a very different beast. It’s a type of protein known as a transcription factor, responsible for sitting on special stretches of DNA next to genes and switching them on. To do this it needs to be very flexible, buddying up with another factor called MAX (or one of a range of other partner proteins) and moulding into the right shape to nestle into DNA’s double helix wherever it’s needed.
Dr Martin Drysdale, head of the Drug Discovery programme at our Beatson Institute in Glasgow, describes MYC as being “like a disordered strand of spaghetti – it has no defined shape until you attach it to MAX or another partner. And there was always this feeling that targeting transcription factors like MYC was difficult, because people have tried to find things in the past and been singularly unsuccessful.
“It comes down to the complexity of how they work from a biological point of view, but also a lack of information about their shape, and how drugs might interact with them.”
What’s clear after several frustrating years is that our methods of finding cancer drugs – either trying to design a molecule to slot into a pocket in a target, or looking at thousands of different chemicals to find ones that fit – simply aren’t working for MYC.
It’s time for some completely new ideas.

Fresh thinkers needed
 “In terms of thinking about the MYC Grand Challenge, what we’re really looking for is innovation in drug discovery,” explains Professor Jones. “People coming together – people who don’t necessarily work on MYC, but who have an interest in drug discovery in general, and thinking about the ways in which we could develop drugs against proteins that are difficult to target in the conventional way.
“In terms of thinking about the MYC Grand Challenge, what we’re really looking for is innovation in drug discovery,” explains Professor Jones. “People coming together – people who don’t necessarily work on MYC, but who have an interest in drug discovery in general, and thinking about the ways in which we could develop drugs against proteins that are difficult to target in the conventional way.
Nobody has been able to do this before. If it’s successful, it will be transformational
Professor Nic Jones
“If we get a consortium that comes in and says ‘we’re going to look at a ‘library’ of small chemicals’, well, that’s not going to fly because it’s been done and it doesn’t work. It’s got to be different, and it’s got to be new.”
There are a few interesting approaches that might work. For example, Drysdale is searching for drugs against a similarly ‘undruggable’ target called RAS, looking for tiny fragments of chemicals that stick to it. Could a similar tactic work for MYC?
Biological molecules such as antibodies – highly specific target-hunting molecules generated by immune cells – could be interesting too. As we explain in this post about our new lab in Cambridge, researchers are ‘fishing’ for antibodies that recognize rogue molecules involved in driving cancer, with the hope of finding future cures. So maybe a fishing trip with MYC could be a good idea.
And MYC doesn’t even have to be the main target either. There could be benefits to targeting MYC’s molecular partners or components of the cellular processes and pathways it’s involved in, whether with conventional drugs, antibodies, or entirely new approaches.
What’s more, according to Jones, solving the problem of drugging MYC could reap much wider benefits for cancer patients in the future. “There are good reasons why we’ve chosen MYC, but we hope that we’ll stimulate ideas that could be applicable for other undruggable molecules.”
He’s convinced that targeting MYC is a tough but achievable task, making it eminently suitable for a Grand Challenge. “I think the simplicity of it, the clarity of it and the potential to benefit patients in a reasonable timeframe makes it a very attractive challenge.
“Some people might think that because it’s such a specific question it’s not that big. But nobody has been able to do this before.
“If it’s successful, it will be transformational.”
The patient perspective
I was part of the Edinburgh Big Think and it was a tremendous experience to be involved in finding the questions that need answering. The interaction and coming together of ideas was amazing and it was obvious that many of the researchers from different disciplines had not had previous contact and this was a new way of working. I came away from the event feeling enthused and applied to be part of the patient advisory panel.
Although I have never taken part in a clinical trial, since my diagnosis with breast cancer in 2004 I’ve come to realise the importance that research played in determining the treatment I received. Being involved in the Grand Challenge is my way of giving something back, helping to improve prevention, diagnosis and treatment for others.”
– Margaret, member of the Grand Challenge patient panel
Comments