A new paper published in Genome Medicine today describes research with the potential to ‘personalize’ treatment for patients with heart disease.

Determining whether or not certain treatments or interventions are right for a particular patient is a tricky business. Much of the time it is about weighing up the benefits versus potential side effects which may be unpleasant for the person being treated. It can ultimately be a matter of life and death.
Personalizing treatment for patients is now talked about for many different conditions, from cancer to arthritis, from heart disease to dental cavities. In essence, and as I’m sure most readers can glean from the name, it entails making treatments more tailored to the individual. In theory, it takes away some of the risk in the decision on whether or not a patient will benefit from a treatment.
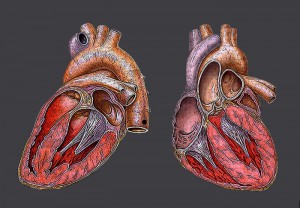
Stratifying patients at risk of heart attack
Despite challenges, progress towards personalized medicine is coming on a pace, as a new paper published today in Genome Medicine shows. In this particular paper, the authors have discovered a genetic signature which could help to stratify patients with coronary heart disease.
By analyzing blood samples, the researchers discovered that patients at significant risk of having a heart attack or dying from a cardiovascular condition showed a particular gene expression ‘signature’.
Specifically, they found gene expression patterns suggestive of down-regulated T-cell signaling and up-regulated inflammation in association with heart attack, and a subset of 200 or so of these genes that were also elevated in 31 people who subsequently died of an acute cardiovascular event.
So what does this actually mean for patients?
“We envision that with our gene expression-based marker, plus some biochemical markers, genotype information and family history, we could produce a tiered evaluation of people’s risks of adverse coronary events,” said Gregory Gibson, director of the Center for Integrative Genomics at Georgia Tech and one of the study’s senior authors. “This could lead to a personalized medicine approach for people recovering from heart attack or coronary artery bypass grafting.”
Given that each year there are around 7.5 million deaths worldwide that can be attributed to coronary heart disease, these findings could have an impact on a huge number of lives.
Personalized vs. stratified medicine
The term ‘personalized medicine’ is now used widely to refer to ways of identifying individuals with certain characteristics who will benefit more from a certain treatment than others without those characteristics. In reality, this is probably better referred to as ‘stratified medicine’ as we’re still identifying groups of individuals with particular characteristics, rather than basing the treatment on one person’s individual ones.
Stratified medicine is not new and there are a variety of examples of it in use in medicine today. Perhaps one of the most well-known is Herceptin – a drug used in breast cancer treatment – which is only given to patients whose cancers test strongly for an unusually high expression of the HER2 protein.
Personalizing treatment for individuals is a step further on from this, looking at ways we could analyze the genes or other characteristics of one particular person to find the most appropriate way of treating them. For example, using the cells of a particular patient to produce a vaccine specific to them.
Why bother?
Whether you use the term ‘personalized’ or ‘stratified’, this idea of narrowing down treatments or interventions to those that will be beneficial for a particular patient, or group of patients, is largely positive.
It means that patients will be getting treatments that are more likely to be effective for them, while others are avoiding treatments that will probably not work for them (and could give them unpleasant or harmful side effects into the bargain).
So far, so simple. But of course things are never quite that straightforward. In a review published in BMC Medicine last year as part of their article collection on personalized medicine, Brian Godman and colleagues summed up some of the issues succinctly:
“[Personalized medicine’s] promise has not always translated into improvements in patient care due to the complexities involved. There are also concerns that advice for tests has been reversed, current tests can be costly, there is fragmentation of funding of care, and companies may seek high prices for new targeted drugs.”
The future of medicine?
It seems clear from recent research trends into genetic indicators and biomarkers that the drive towards personalized medicine is gaining momentum. According to Godman et al. there “should be considerable benefits to all key stakeholders, with new technologies that improve the diagnosis, prognosis and treatment of patients.”
So what about this latest research in Genome Medicine? Author on the paper Gregory Gibson has a clear vision for where their findings could lead:
“Our dream would be a hand-held device that would allow patients to take a droplet of blood, much like diabetics do today, and obtain an evaluation of these transcripts that they could track at home,” he said. “If we can use this information to help people adopt healthier behaviors, it will be very positive.”
Comments