 Recent research published in Genome Medicine presents a comprehensive, global view of lipid abnormalities associated with schizophrenia, providing new pathophysiological insights into the disorder.
Recent research published in Genome Medicine presents a comprehensive, global view of lipid abnormalities associated with schizophrenia, providing new pathophysiological insights into the disorder.
Following on from their earlier work published in Genome Medicine, which reported metabolites that differentiate schizophrenia from related disorders, Matej Orešič and colleagues from the VTT Technical Research Centre of Finland used metabolomics (a high-throughput method for detecting small metabolites) to determine the lipid profile of people with schizophrenia. In psychiatric research, several theories have been proposed to explain how brain function may be altered by changes in lipid composition, and this study sought to understand which specific pathways are affected in schizophrenia.
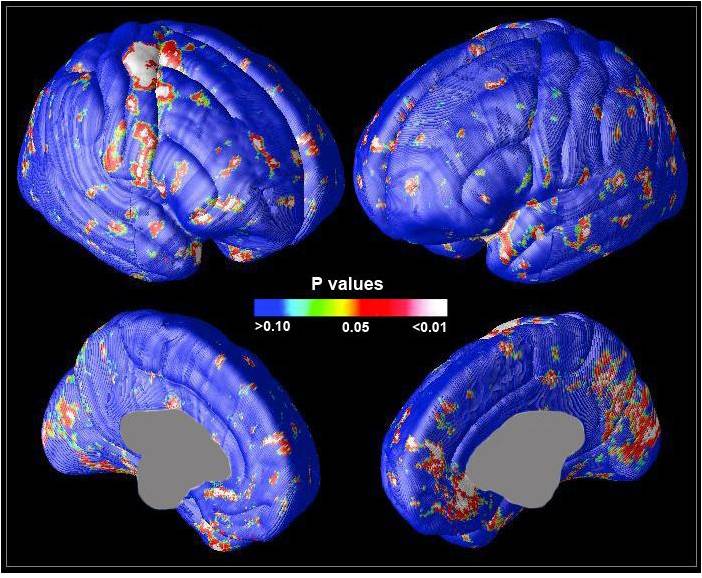
The group analyzed the lipid content of serum samples taken from monozygotic twins that are discordant for schizophrenia i.e. only one twin in each pair is affected. The advantage of this unique study design is that discordant twins are an ideal population for investigating the contribution of genetic factors to disease etiology. Age and gender matched healthy twin pairs were included as controls, and neurocognitive and magnetic resonance image data were available for selected twins.
Compared with healthy controls, individuals with schizophrenia had higher triglyceride levels and showed signs of insulin resistance, in line with earlier reports. However, the patients’ unaffected co-twins were also found to be insulin resistant, providing new evidence that this could be an inherited trait associated with predisposition to schizophrenia. Affected twins also had lower levels of phospholipid derivatives called lysophosphatidylcholines (lysoPCs). This change, which was not observed in healthy co-twins or controls, correlated with decreased cognitive speed. Because lysoPCs are involved in blood-brain barrier transport of polyunsaturated fatty acids, the authors conclude that a drop in their levels may be responsible for changes in neurotransmission and weaker cognitive performance. They also propose that lysoPC deficiency could make schizophrenia patients more susceptible to infections. These findings pave the way for further research into the role of lysoPCs in schizophrenia.
The mechanistic insights reported by Orešič and colleagues may be useful for the discovery of new drug targets for schizophrenia. In addition, the work demonstrates how a discordant twin study design can successfully uncouple genetic and environmental factors, allowing disease-specific inherited traits to be accurately defined.
Comments