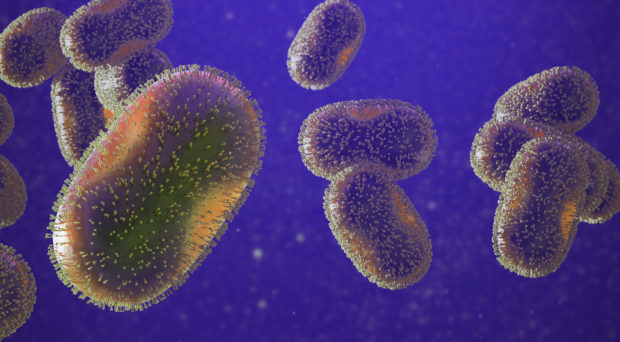
An unusual Monkeypox outbreak has emerged and been reported in over 59 non-endemic WHO member countries with more than 6,027 laboratory confirmed cases. Human infections with the central and West African clade, namely the Congo Basin clade in Cameroon, Nigeria, DR Congo, CAR, South Sudan and the Great Lakes, appear to be less severe, with fatality rates in other African countries of 3.6% and 10.6% in 2017, associated with children and babies to untreated HIV or compromised Immunodeficiency patents. The geographical distribution showed the majority of cases in WHO European regions (n=2933, 86%) and the American region (n=381, 11%), eastern Mediterranean (n=15, <1%) and western Pacific (n=11, <1%). However, no case of death has been reported from ongoing Monkeypox outbreaks in non-endemic countries so far, and eight endemic African countries have had 73 confirmed cases and three death recorded in Sub-Saharan Africa (WHO, 2022). Prior the current outbreak, endemic African countries have reported 1365 cases and 67 deaths due to the same virus from mid-December to late May 2022 (WHO, 2022).
The disease can be transmitted directly or indirectly through contact with infected skin lesions in contaminated patients, shared towels and bedding. Typical symptoms vary from fever, aches, and myalgia to intense headache, lymphadenopathy and skin eruption. Ongoing epidemiological investigation reported that most cases are linked to travel history, sexual health behaviour and heterosexual contacts or other indirect/direct contacts in households and healthcare facilities. Yet, non-travel reported cases are atypical and could serve as outbreak alertness and in strengthening of International Health Regulations (IHR, 2005) and global health security measures (WHO, 2022).
Mass Gatherings during Pandemics
Two major mass gathering events will be taking place in Gulf countries. The Hajj 1443H and Umrah 2022 is slated to have 1 million international and local pilgrims in Saudi Arabia, and the Qatar FIFA World Cup 2022 will also attract many travelers.
Noting the absence of regular and sustained surveillance and monitoring mechanisms in both endemic and non-endemic countries, the syndemic of COVID-19 pandemic and Monkeypox epidemic could cause more significant health, socioeconomic and global health security consequences. We urgently call for action by governments to rapidly strengthen and implement Monkeypox CDC outbreak preparedness and response actions plans in both non-endemic and endemic countries.
What Should Be Done?
These innovative public health preparedness and response actions against Monkeypox outbreak amidst the COVID-19 pandemic include:
- Scaled-up local and global information sharing, awareness and travel guidance.
- Enhanced point of entries and systemic infectious disease outbreaks surveillance monitoring systems.
- Boosting pilgrim and tourist travel-related information and quarantine measures regularly.
- Promoting and sustaining local and international risk communication and community engagement.
- Scale diagnostic, enhanced genomic surveillance for rash-like illnesses and comprehensive case finding and contact tracing at all levels, mainly healthcare delivery services sites.
- Improving clinical management with supportive care as well as communities’ resilience building amongst at risk countries and vulnerable groups.
- Addressing the local and global impact of increasing climate change and global trade/travel effects on scale and spread of outbreaks and pandemics.
Mass gathering engagement and outreach should consist mainly of national health education and awareness outreach on emerging Monkeypox illness, coupled with COVID-19 preparedness and response trainings and capacity building. Monkeypox vaccination programs should be implemented at point of entries, as well as effective strategies to mitigate social media rumors and misinformation in order to prevent and control the growing public and global health menace.
Promoting prompt, reliable and secured information sources ought to continue to raise citizen and country readiness by governments and stakeholders to prevent, monitor and tackle any eventual outbreak of Monkeypox in mass gathering and healthcare settings. More efforts are required in increasing/improving integrative ‘One Health’ approach outbreak risk communication and community engagement in affected countries, in order to detect, prepare and prevent at-risk populations, pilgrims, tourists and footballers, and respond to such unprecedented global outbreak threats and effects on travel medicine and global health security under International Health Regulations (IHR), 2005 (WHO, 2022).
Interestingly, smallpox vaccines have shown to be effective at providing herd immunity against this Monkeypox virus, but this requires more extensive research in building targeted population based efficacy and safety evidence for comprehensive and sustainable decisions policies, recommendations, and response actions. Addressing knowledge gaps and research priorities to improve available vaccines effectiveness and safety evidence is paramount to build effective and sustainable countermeasures and immunization responses. Strengthening local and global ‘One health’ approach implementation research, collaboration and importations/trade control measures is crucial in understanding and addressing animal reservoirs-human and environment transmission dynamics and spread, to encourage better diagnostics and interventions, hospital prevention and control best practices.
Both authors have no conflict of interest.
References
- WHO, 2022 (accessed 09/July 2022). Multi-country monkeypox outbreak: situation update (who.int)
- CDC, 2022 (accessed 04/June 2022), S. Monkeypox Outbreak 2022: Situation Summary | Monkeypox | Poxvirus | CDC
- WHO monkeypox research: what are the knowledge-gaps and priority research questions? WHO monkeypox research: What are the knowledge gaps and priority research questions?
Comments