Although control measures have successfully reduced the burden of schistosomiasis in some countries in recent years, the complexity of transmission in many settings requires interdisciplinary research and integrated interventions.
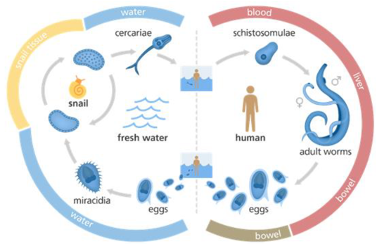
Breaking the transmission of schistosomiasis can focus on several parts of the parasite’s life cycle. The current mainstay of control in endemic countries is annual mass drug administration (MDA) with praziquantel, targeting adult worms in an infected person and therefore reducing the egg production and onwards transmission. Other control measures include safe water supply (reducing risk of infection through infested water contact), adequate sanitation (reducing the risk for excreted eggs to reach the water to hatch), behavior change (improving water and sanitation practices as well as MDA uptake and health seeking behavior) and vector control (reducing the amount of intermediate host snails). Each of these control measures comes with opportunities and challenges such as efficacy, feasibility, acceptability and cost. And as one of the neglected tropical diseases, schistosomiasis is not often at the top of the global health agenda, even further challenged by several public health resources being re-allocated to the COVID-19 pandemic in recent years.
Due to these challenges in control of transmission and disease, areas with persistent high endemicity can remain. This phenomenon can be attributable to untreated individuals but even in areas with high MDA coverage, treatment does not prevent reinfections. Identifying factors driving reinfection as well as factors protecting people from infection in hotspots is a complex challenge but could provide helpful insights towards control in these areas.

By using a mixed methods approach combining epidemiological, ethnographic and malacological methodology we aimed to better understand water contact behaviours and their interplay with infection risk in an area with persistent high endemicity in Uganda.
We used repeated parasitological surveys to survey a small group of school-aged children. We showed that although some children were repeatedly infected with schistosomiasis, reaching moderate infection intensities only 3 months after treatment and observed clearance, other children had no infections or very low-intensity infections. This is surprising, as they all lived in close proximity to water bodies where the intermediate host snails were present. Building on these quantitative findings, we used qualitative methods to better understand reasons driving this difference.
Through focused ethnographic observations of the same children included in parasitological surveys, we found that water contact happened frequently, including for domestic, personal care, recreational, commercial and religious purposes. Contact occurred directly at various water sources but also indirectly with previously collected water. These water contact activities occurred both in children that were not infected and that were rapidly reinfected. However, children that were rapidly reinfected were uniquely observed to swim in the lake, fetch water for other households in exchange for money and skip school. Children had more water contact on days when they were not in school. Households of children that were not infected were more likely to collect rainwater, an alternative source of water safe from schistosomes.
During observations, we noted specific locations where children contacted water. All of these sites were then surveyed for intermediate host snails four times over a year and collected snails were checked for schistosome infections. We found that rapidly reinfected children went to a larger variety of water contact sites and also frequented sites with specific snail species. We also observed that these children contacted water more frequently during midday when snails are reported to shed more parasites. Although we didn’t find many schistosome-shedding snails, we found a large abundance, particularly in the dry season.

Control programmes focussed on MDA do not address all the complexities of schistosomiasis infection and additional efforts are needed to work towards the target of eliminating schistosomiasis as a public health problem by 2030. We used a combination of approaches to confirm findings, target data collection, and identify new interlinked results. Although using mixed methods can be challenging, requiring a range of skills, overcoming disciplinary differences and often additional resources compared to mono-method research, interdisciplinary research on such complex issues can offer more complete, balanced and robust perspectives and provide useful recommendations for much-needed integrated control measures.
Let’s work together to make a disease that has plagued humans for thousands of years finally come to a halt.

Comments