
Schistosomiasis control and elimination as a public health problem
Schistosomiasis is an endemic parasitic disease affecting over 200 million people. It is treated with praziquantel through school-based and community-wide mass drug administration programmes. The World Health Organization (WHO) has recommended treatment guidelines to achieve the following goals:
- morbidity control: reducing the prevalence of heavy-intensity infections in school-aged children to ≤5%
- elimination as a public health problem: reducing the prevalence of heavy-intensity infections in school-aged children to ≤1%

Monitoring and evaluation (M&E) activities are used to collect data which are required to inform and assess treatment strategies for schistosomiasis.
Due to programmatic and financial constraints, treatment is specifically targeted at school-aged children (SAC; 5-14 years old) as they are most likely to be infected. Additionally, as SAC are relatively easy to sample, M&E activities typically collect infection data from this age-group. However, adults may also form a large proportion of those infected.
The Neglected Tropical Disease Modelling Consortium
The Neglected Tropical Disease (NTD) Modelling Consortium aims to develop mathematical models of NTD transmission dynamics and the impact of control measures. Multiple groups work on each disease to increase robustness of modelling results. The consortium focuses on infections included in the London Declaration on NTDs, such as schistosomiasis.
Within our work, we have developed mathematical models of schistosomiasis transmission dynamics and treatment impact to assess the effectiveness of current WHO treatment guidelines and M&E activities (with a focus on intestinal schistosomiasis caused by Schistosoma mansoni and prevalence measured by the Kato-Katz diagnostic technique).
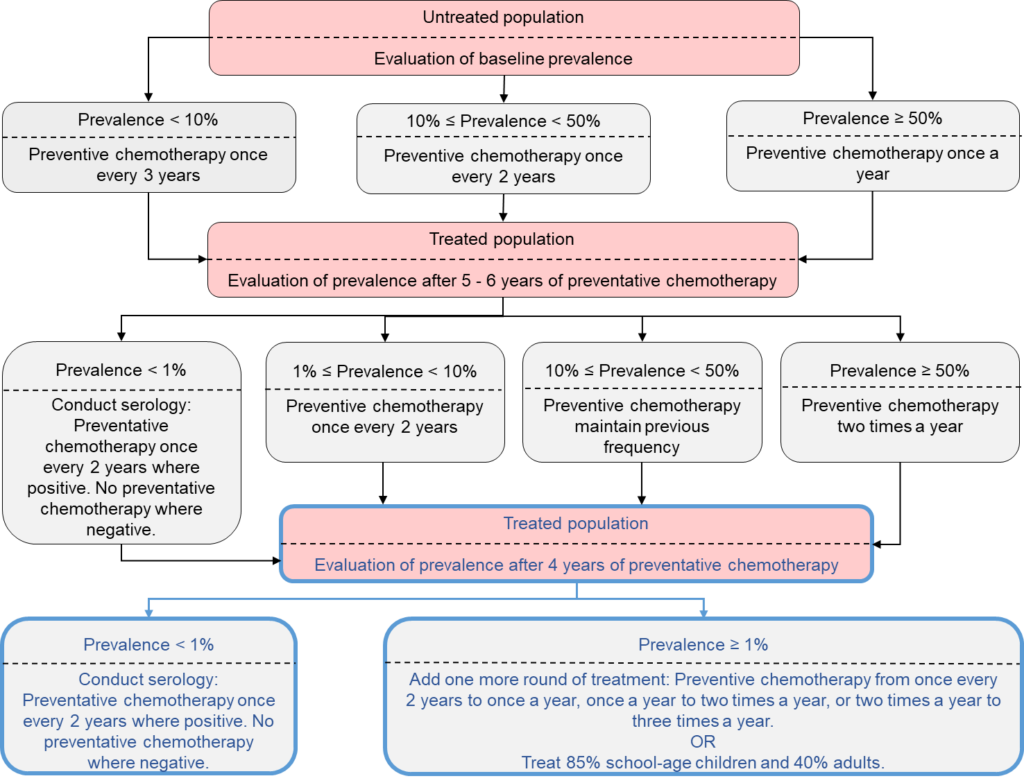
Treatment guidelines
Current WHO guidelines generally focus on treating 75% of SAC at a treatment frequency determined by the prevalence of infection in SAC. Using our models, we simulated settings with low to high prevalence levels and then implemented the recommended guidelines. Our analysis showed that in low (<10%) prevalence settings, treating 75% of SAC only is likely to reach morbidity control and elimination as a public health problem. However, in moderate to high (≥10%) prevalence settings, treatment coverage levels need to be increased and expanded to at least 85% for SAC and 40% for adults in order to achieve these goals.
Monitoring and Evaluation activities
To determine whether the burden of infection in adults will impact the treatment strategy required to reach morbidity control and elimination as a public health problem, different age-intensity profiles of infection were incorporated into the model. The age-intensity profiles corresponded to low, moderate and high burdens of infection in adults relative to SAC. Our analysis showed that in moderate prevalence settings data from SAC-only is sufficient. However, in high prevalence settings, data needs to be collected from adults, as well as SAC. Here, treatment of SAC and adults is required to reach the WHO goals, with coverage levels varying with the burden of infection in adults. Hence, the optimal treatment strategy requires consideration of the burden of infection in adults as it cannot be based solely on the level of infection in SAC.
Policy impact
Currently, there are ongoing discussions on improving the WHO treatment guidelines and M&E activities for schistosomiasis. Our modelling work has provided a vital insight into how we can successfully achieve the WHO schistosomiasis goals. We have highlighted the importance of treating and monitoring adults as well as SAC within the schistosomiasis community.
There is more policy-driven research to be done on schistosomiasis, including modelling with different diagnostic techniques and other schistosome species. By conducting this research, we hope to continue providing insight for the discussions on what the future WHO schistosomiasis guidelines and M&E activities should be.

Comments