Schistosomes and Schistosomiasis
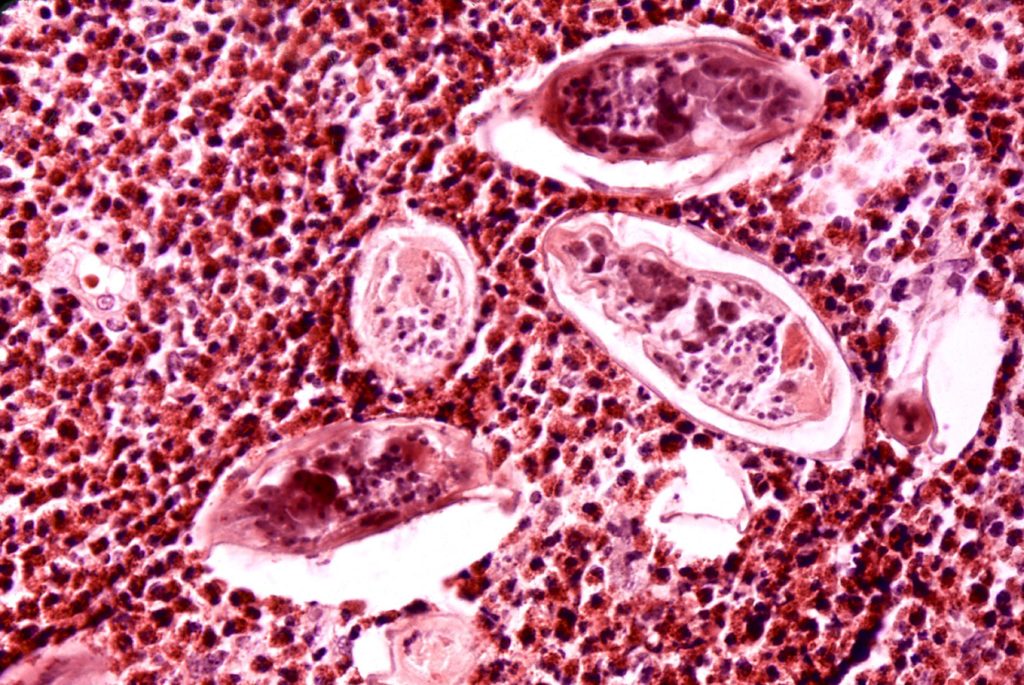
Schistosomes live in the blood system of mammals, they produce hundred to thousands of eggs per day that break through the barrier between the blood system and the urinary or intestinal tract (depending on the schistosome species) to exit the body when the host urinates or defecates. But it is estimated that at least a third of the eggs do not make it out of the body and instead get washed up into organs. This is where the danger lies. The trapped eggs lead to damaged tissues, damaged organs and an increasing risk of severe and life-threatening conditions.
The damage caused by these parasites is severe but the chronic nature, spectrum of disease manifestations and complex epidemiological settings presents challenges to its diagnoses, control and elimination in resource-poor settings where it is prevalent.
Uro-Genital Schistosomiasis
Schistosome eggs are dispersed through the venous system and can lodge in various organs, leading to granulomas and tissue damage. S. haematobium eggs often end up in the urinary and reproductive organs causing inflammation and lesions. When the eggs lodge in the genital tract they cause a form of the disease called genital schistosomiasis. In women, where the impact is more apparent, this is called female genital schistosomiasis (FGS). In men it is called male genital schistosomiasis (MGS).
The WHO estimate that approximately 56 million women suffer from FGS.
Symptoms of genital schistosomiasis include:
- Blood in urine (haematuria)
- Abdominal and pelvic pain
- Pain with coitus (Dyspareunia)
- Post-coital and contact bleeding
- Vaginal discharge
- Dysuria (pain or difficulty urinating)
- Inflammation of the cervix, endometrium layer and/or of the fallopian tubes
- Inflammation of the skin around testicles (Epididymitis)
- Male chronic pelvic pain syndrome
- Painful erection and ejaculation
- Blood in semen (Hermatospermia)
- Glandular tumours near the prostate (adenomcarcinoma)
Potential complications from genital schistosomiasis include miscarriages, ectopic pregnancy and infertility. These not only carry huge risks to women but their impact on mental health and social status cannot be underestimated. Infertility can be a taboo subject in many cultures and can lead to a broader range of issues such as stigma, economic difficulties and social exclusion and isolation.

Link with HIV
Researchers have shown that there is a strong association between FGS and HIV infections, in fact women with schistosome infections are potentially far more susceptible and at an increased risk of HIV. A causal link has not yet been established but the evidence is strong and further research by way of a clinical trial is being undertaken (see below under Prevention)
The pathology of genital schistosomiasis is like many sexually transmitted diseases and when patients present themselves to a local health facility with these symptoms they are often misdiagnosed by healthcare professionals due to the lack of awareness and clear diagnostics. Thus, patients often receive the wrong treatment and are said to be non-responsive to treatment or as having “chronic pain”. Either way their misery is not alleviated.
Diagnostic challenges
The problem with diagnosing genital schistosomiasis is linked to the general problem of diagnosing schistosome infections. We still rely on microscopic identification of schistosome eggs in urine and stool samples as the gold standard. We already know that this is not an ideal diagnostic since there is variability in egg production and excretion and light infections are often missed. A complication for genital schistosomiasis is that once established the lesions and tissue damage last after worm infections have been resolved (whether through treatment with Praziquantel (PZQ) that kills adult worms or from the natural death of the worms themselves).
Thanks to researchers and the WHO we now have a WHO Atlas for FGS, an imaged based reference guide for the diagnosis of FGS in clinical settings.
However, this has to used with other screening methods to make sure that other infections and diseases have been ruled out (STIs, urogenital TB, cancer screening). Plus, this image based atlas can only diagnose schistosomiasis in the lower genital region of the female reproductive tract and may miss damage to the fallopian tubes.
Another problem is that these clinical diagnostic methods require the use of specialised equipment such as a colposcope, and highly trained personnel which can be challenging in the resource poor settings where schistosomiasis thrives.
Another possibility is the use of molecular techniques based on the identification of schistosome DNA in the genital tract. A study currently being undertaken in Zambia is looking at a potential home-based self-screening test for the detection of S. haematobium DNA as a proxy to FGS diagnosis. It is also testing the applicability of an affordable point-of-care colposcope the size of a smart phone that can be operated by non-highly skilled personnel. This device is already deployed for the diagnosis of cervical cancer in low resource settings.
Further research is needed to refine and develop practical and scalable diagnostic techniques for genital schistosomiasis in resource poor settings. This needs to be combined with further research on the pathological pathways of schistosome infections in the reproductive tract of humans.
Treatment
What if we had an easy to use diagnostic test, or a highly trained clinical nurse used the WHO FGS atlas to successfully diagnose a woman with Female Genital Schistosomiasis? We would of course treat them with the known available drug effective against all schistosome species, Praziquantel. But here is the bad news. The evidence indicates that giving PZQ at it’s current recommended dosage of 40mg/kg is not an effective treatment for FGS. It can kill living adult worms still residing in the blood vessels, but it is not effective at reversing already established lesions and tissues damage.
This is devastating news for the millions of women who already have FGS. We urgently need an effective treatment to reverse FGS lesions and tissue damage. A potential solution might be found in PZQ itself. It does after all have anti-inflammatory properties therefor perhaps at a higher concentration it might reverse some of the damage already established from FGS.
This surely needs to be pursued and quickly in order to provide some relief to those with genital schistosomiasis.
Prevention
The good news is we can prevent FGS and MGS from developing! And we do. Cross sectional studies have shown that women coming from areas where schistosomiasis control programmes using preventative chemotherapy with PZQ have been in place are significantly less likely to have FGS outcomes and receiving PZQ treatment before the age of 20 is significantly associated with the absence of FGS.

Currently a clinical trial is underway in South Africa to see if regular PZQ treatment in pre-pubescent and post-pubescent young girls can prevent FGS and HIV infections.
We are eagerly awaiting the results!
Male Genital Schistosomiasis
FGS currently gets a bit of attention, although in this author’s humble opinion not nearly as much as it should be getting! However, MGS is severely neglected. Cross-sectional studies have shown that schistosome eggs are present in semen indicating that there could be a high number of eggs lodged along the reproductive tract of men causing tissue damage and problems. More research is underway but we need more surveys and clinical trials to better understand the impact of genital schistosomiasis on men.
Next steps
The WHO and UNAIDS are calling for more research on diagnosis, link with HIV, and large-scale coverage of schistosomiasis treatment.
Uniting to Combat NTDs, the advocacy group for all 10 NTDs targeted by the London declaration (covered by a previous blog) recently produced a policy document to raise awareness of FGS and how NTD control programmes can prevent this disease from developing.
But PZQ administration through preventative chemotherapy is currently focused on primary schools. What about secondary schools and adolescent children? What about mothers and pre-school aged children? How about distributing Praziquantel in sexual and reproductive health clinics?
We need:
- Research for better practical diagnostics for female genital schistosomiasis.
- Clinical trials to strengthen the evidence of a causal link between FGS and HIV to help us engage and advocate for the inclusion of schistosomiasis in already established HIV/AIDS and reproductive health programmes and clinics.
- An effective treatment for the millions of women already suffering from established genital schistosomiasis and
- Research to better understand the impact of male genital schistosomiasis.

For more info on FGS read the International Society for NTDs briefing on FGS, FGS workshop presentations, a recent review on FGS and the BRIGHT website

Comments