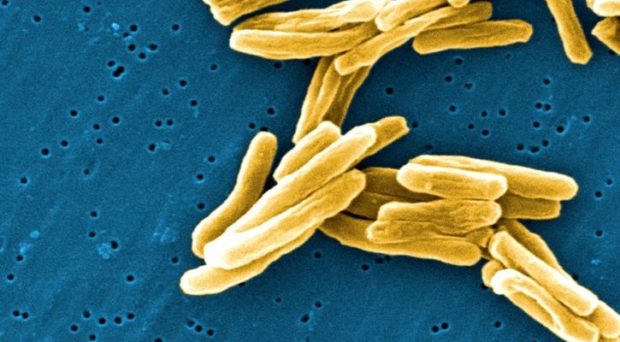
The global tuberculosis (TB) control community is in a challenging situation. With the number of deaths from TB overtaking HIV in 2014 to make it the leading infectious disease killer in the world, the contrast between gains made against HIV and TB is apparent.
Questions are being raised about why TB control strategies have been unable to manage a disease that has been around for over 20,000 years, despite robust evidence about effective interventions from decades of research, and availability of cheap treatment for the past 60 years.
Those of us fighting to defeat TB argue that funding is a key factor in all of this. An analysis of research investments for UK institutions between 2011 and 2013, for example, showed that TB research received half as much as HIV and malaria.
An analysis of research investments for UK institutions between 2011 and 2013 showed that TB research received half as much as HIV and malaria.
There is no question that a dramatic shift in approach is needed. If we keep going as we are – with global incidence declining just over one percent per annum – it will take more than 150 years to meet the 2035 End TB targets of reducing deaths by 95% and incidence by 90%.
There is also wide consensus that the barriers to controlling TB are numerous, including its association with poverty and the generation of drug resistance owing to inadequacies in health systems. However, since challenges are fairly well defined, the question is whether new calls for action direct researchers to look for innovative solutions while neglecting to act effectively on the basis of existing knowledge.
In a recent paper published in BMC Medicine, we examine two critical gaps for TB control: in funding, and in evidence owing to essential research being left off the priority agenda.

Gaps in Funding
The Global Plan to Stop TB 2011–2015 set a target US$10 billion for Research and Development (R&D) across five key areas: drugs, basic science, vaccines, diagnostics and operational research. Overall, global spending on TB R&D fell far short of this; by the end of 2014, only $2.7 billion, just over one-fourth of the target, had been invested.
The scarcity in funding was not equally felt across research areas, however. A comparison across the five R&D areas in 2014 demonstrates that both targets and actual investments were heavily skewed towards two research areas: drug discovery and basic science. With a target of $1.16 billion for 2014, these two areas accounted for 60% of recommended annual R&D funding. Of the $674 million actual R&D investment in 2014, these areas received 58%.
We therefore spent $570 million on research to develop new drugs, vaccines and diagnostics and less than 10% ($53 million) on overcoming critical barriers to implement new and existing tools.
Not surprisingly, this funding distribution adds fuel to the fire of those emphasising that too much is spent on generating new tools and too little on understanding how to apply the ones we have.
The 2011-2015 Global Plan did, for the first time, include operational research as a distinct area, recognising its essential role in ensuring uptake of new tools and efficient implementation of existing strategies. However, the funding target for operational research represented only 4% of the total target.
We therefore spent $570 million on research to develop new drugs, vaccines and diagnostics and less than 10% ($53 million) on overcoming critical barriers to implement new and existing tools.
Gaps in knowledge for impact
Our study also identified additional areas highlighted by researchers that are not on the global research priority agenda at all, through a review of published literature and consultation with researchers across multiple disciplines in the London School of Hygiene and Tropical Medicine TB Center.
These critical research areas included:
- Improved understanding of TB transmission dynamics to plan more targeted, effective prevention interventions
- The role of social protection and social determinants
- Health systems and policy research to inform decision-making and optimal resource allocation by national policymakers
A call to rethink calls for action
While funding priorities are increasingly important in light of resource limitations, we should critically consider what priorities are being set and who is setting them.
While funding priorities are increasingly important in light of resource limitations, we should critically consider what priorities are being set and who is setting them.
Rather than restricting research activities to discrete silos, supporting multidisciplinary approaches that address complex socio-political realities underpinning the success of new tools is essential.
Indeed we could learn lessons from the massive reduction in TB incidence in Europe, which was achieved without drugs, vaccines or technologically-advanced diagnostics.
To ensure that funding allocation better reflects priorities of researchers and TB control programmes in high TB burden countries, platforms that encourage more, and wider, dialogue between stakeholders are essential. A pragmatic solution would the formation of national bodies for research agenda setting to inform global funding priorities and play a role in evaluating potential impact of research proposals.
Comments