
Fever is a common cause of presentation to pediatric emergency departments (EDs), accounting for ~20% of all visits. Most children with fever have self-limiting viral illnesses; however, severe bacterial infections may result in almost identical clinical presentations, making diagnosis a difficult task.
Because of the catastrophic consequences of missing a potentially life-threatening bacterial infection, a cautious approach to the management of the child with fever is often taken, involving extended observation, investigations, and precautionary use of antibiotics, often without definitive evidence of bacterial infections.
The cost of missing cases of serious bacterial infection are significant from a personal, family, societal and resource perspective
These life-threatening infections represent a needle in the haystack, and the challenge for clinicians is to accurately identify children with serious bacterial infection (SBI) early, so that urgent treatment can be administered. The real problem is sorting out the tigers from the pussycats because a baby tiger may be easily mistaken for a pussycat, but once it grows, it develops into a ferocious beast capable of inflicting serious harm.
The judgement is difficult, and often vital clues are missing. With experience, comes increased confidence to make the correct diagnosis, but, even then, there may be a (smaller) probability of errors in clinical judgement. The cost of missing cases of SBI are significant from a personal, family, societal and resource perspective.
The cases of missed life-threatening SBI with catastrophic consequences are the cases we all remember. These are the cases which are reported in the media, and which provoke such fear and anxiety amongst parents and carers.
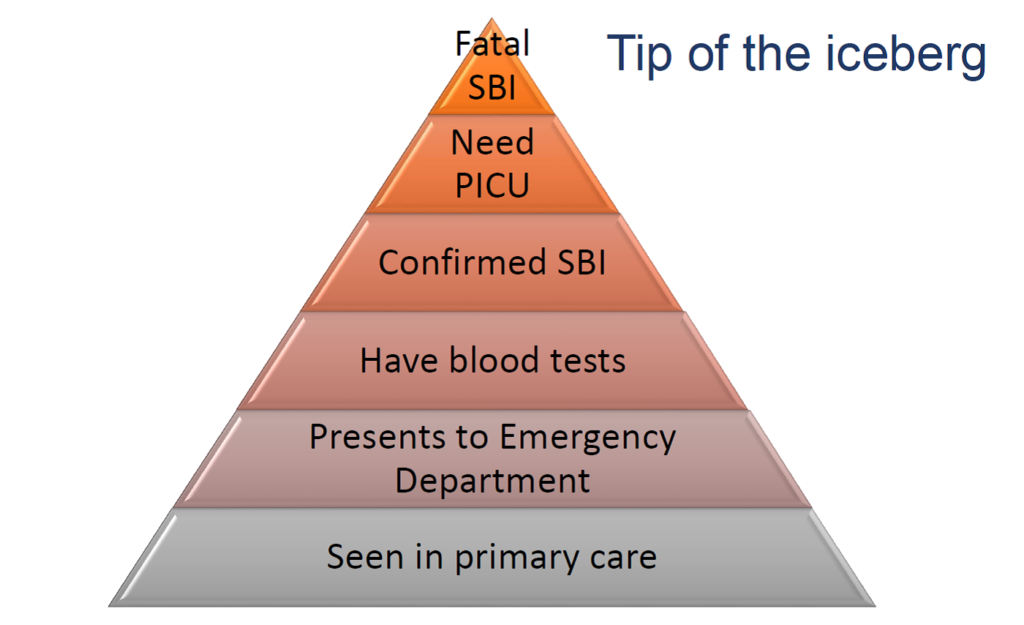
Not surprisingly, doctors working on the frontline, where febrile children are assessed, are also plagued with these fears. Doctors choose a career in medicine because they desire to alleviate human suffering, and the thought of ending up before a tribunal for negligence, is nothing short of a worst nightmare. The reality however, is that fatal SBI represents the tip of the iceberg, yet the fear of this extremely rare event drives a lot of clinician behavior in the assessment of the febrile child.
Diagnosis
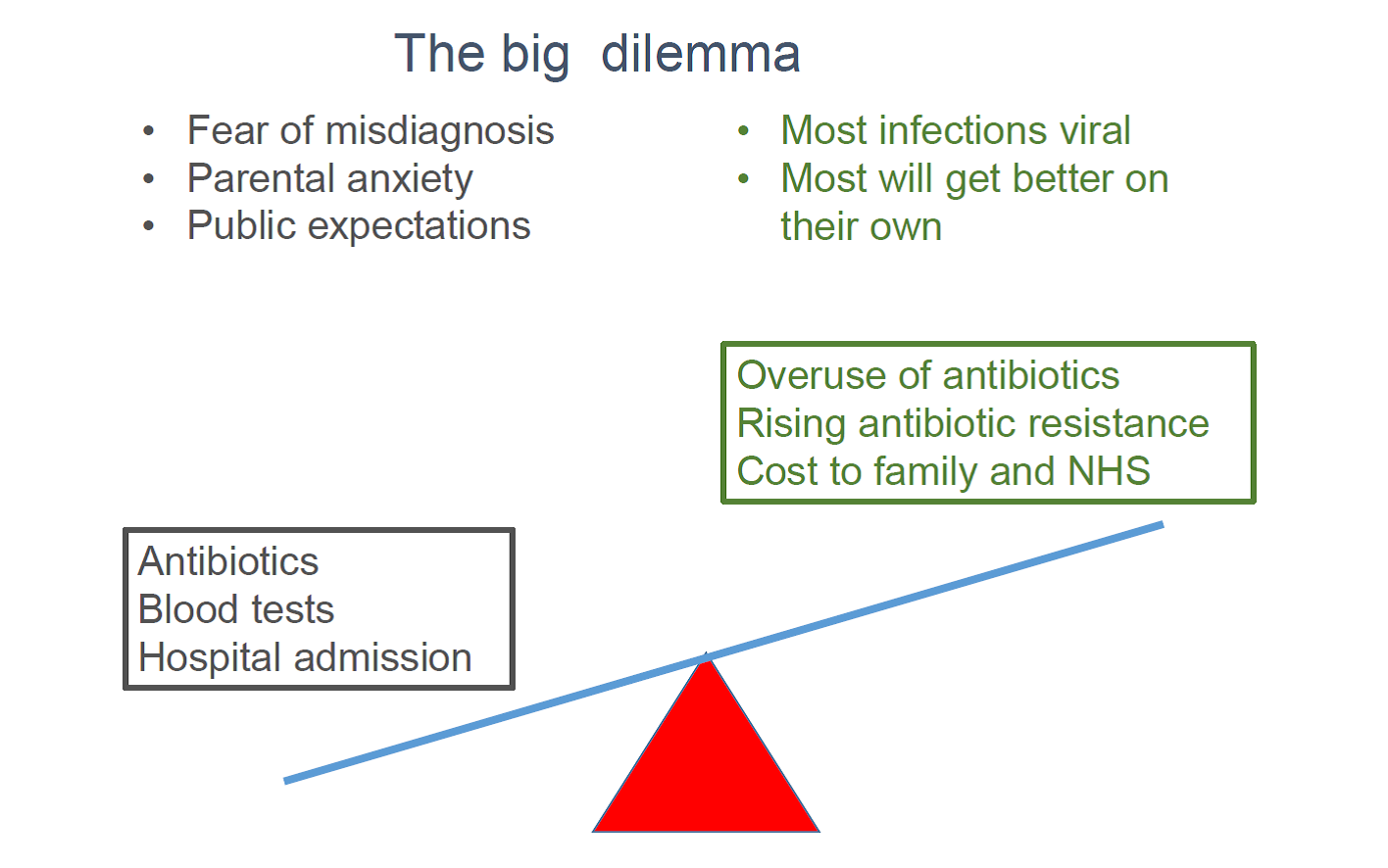
The lack of gold standard diagnostic tests which accurately distinguish SBI from viral infections presents a dilemma for clinicians. On one hand, there is the fear of misdiagnosis, parental anxiety and unrealistic public expectations that doctors should always have the answer. On the other hand, the reality is that most of these febrile illnesses are viral and will get better on their own.
This uncertainty results in a cautious approach, with further investigations, antibiotics “just in case”, and hospital admission for observation with intravenous antibiotics, when uncertainty and risk are perceived to be highest.
Hospital admission is undoubtedly the safest option because any further deterioration will hopefully be monitored and urgent interventions can be instituted. However, this “safest option” is not without consequences: overuse of antibiotics, rising antimicrobial resistance and significant cost to the child, family, society and the NHS.
Increasing efficiency, reducing antibiotic use
In a large, real-life study in Liverpool of over 6500 children presenting to one of the busiest children’s EDs in Europe, we sought to determine the potential economic impact of the diagnostic uncertainty in assessing febrile children. The study collected data on all febrile children presenting to a large children’s ED over a 12-month period. The question we asked was “What difference would it make if there was an accurate and rapid diagnostic test to confidently exclude life-threatening SBI?”.
Antimicrobial resistance is a growing global health crisis which requires urgent collective action. In conjunction with this, initiatives which reduce costs and provide efficiencies are desperately needed, in cash-strapped health systems like the NHS where demand outstrips rising need.
If the cost of the uncertainty is significant, then the message to payers, providers and the diagnostic companies is still relevant. In order to make a difference, in high income countries, the diagnostic test does not need to be cheap; it needs to highly accurate, rapid, easy to use and widely available.
Our study shows that the difference in healthcare resources and costs, between a child with a self-limiting viral illness who receives antibiotics and additional investigations, and a child who does not, is over £1,000. For infants under 3 months, where the risks of SBI are greatest, the difference in spending is even higher at over £2000.
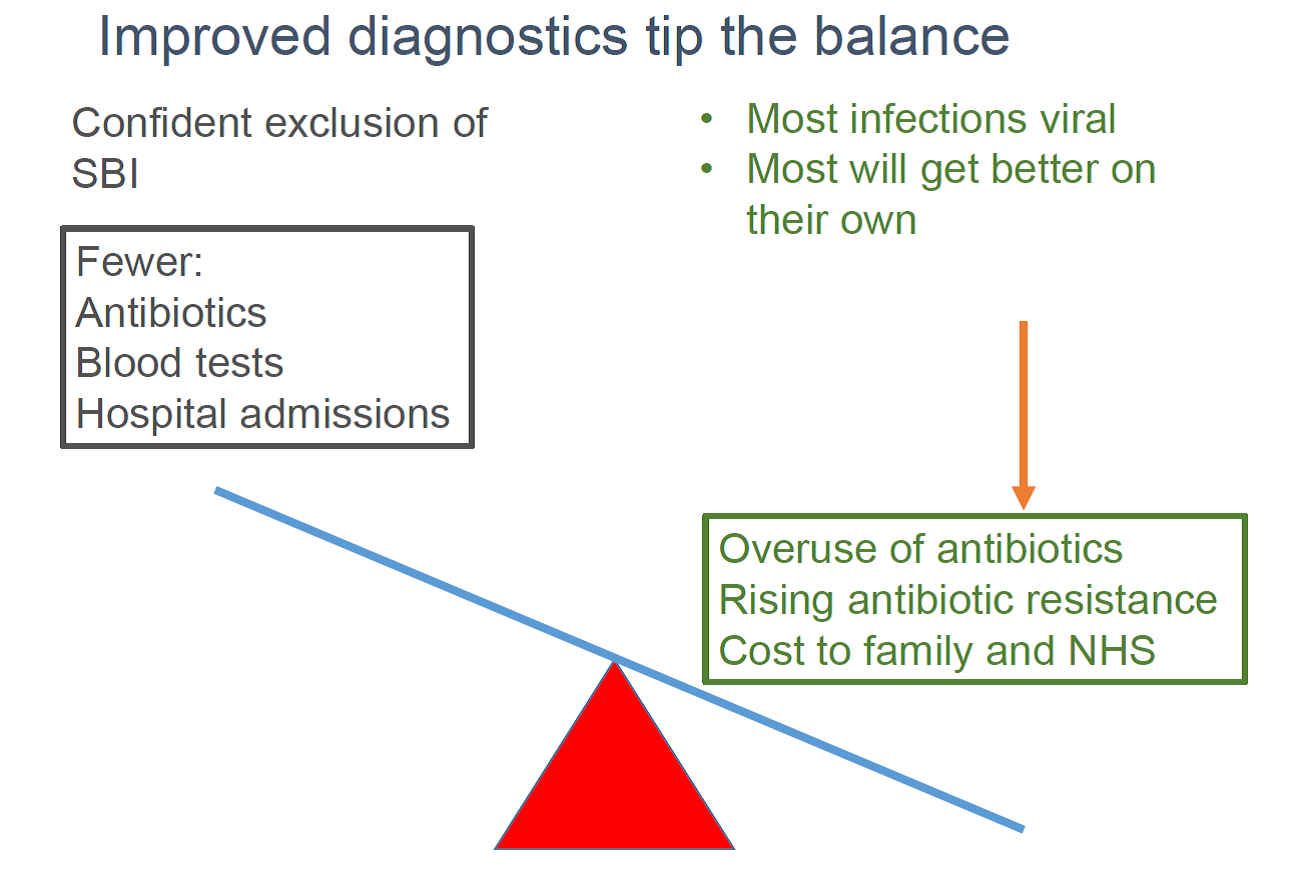
Had an accurate diagnostic test been available, antibiotic use could potentially have been reduced by about 60%
If you scale these figures up to a medium-sized ED that sees 4000 febrile children a year, typical in many parts of England, it amounts to a staggering £1.3 million additional spending per NHS Trust each year. That is enough to fund, for example, an extra 25 band-6 nurses every year.
In addition to reducing costs, had an accurate diagnostic test been available, antibiotic use could potentially have been reduced by about 60%. These figures are startling in an era when rising antimicrobial resistance threatens the core of modern medicine.
The study highlights the role that accurate new diagnostic tests could play in EDs, improving care and convenience for families, not only in reducing unnecessary antibiotic use, but also in improving the efficiency and appropriateness of the NHS services. If new diagnostic tests enable us to target investigations, antibiotics, and hospital beds to those who will benefit most; this frees up these funds to be put to good use elsewhere; while also giving parents reassurance as quickly as possible.
This research was conducted in a high-income country, but this is very much a global problem. New and better diagnostics, especially if they are affordable, will potentially have huge benefits for our health services world-wide, particularly in resource-poor settings, like in sub-Sahara Africa and rural Asia. 21st century global health challenges such as rising antimicrobial resistance cannot be tackled in isolation; they deserve global partnerships, like the PERFORM consortium.
Novel diagnostic tests will help sort out the tigers from the pussycats, increase confidence to withhold antibiotics and investigations, and will yield considerable efficiency gains among those children where the perceived risks of failing to identify potentially life-threatening bacterial infections are greatest.
Comments