Introduction to nasopharyngeal carcinoma
Nasopharyngeal carcinoma (NPC) is a type of head and neck cancer, and usually originates from the top and lateral mucous membrane of the pharyngonasal cavity. It is also referred to as ‘Guangdong tumor’, as 80% of NPC cases occur in China, especially in Southern China, such as the Guangdong, Guangxi, Hunan, and Fujian provinces, with an incidence of 30-50/100,000.
In contrast, NPC is quite rare in Europe and America, with a low incidence of about 1/100,000. Early-stage NPC exhibits atypical symptoms, and more than 70% of the patients usually visit a clinic after noticing a neck mass.
At present, the main treatment of NPC is a comprehensive treatment consisting of chemotherapy and radiation therapy
At present, the main treatment of NPC is a comprehensive treatment consisting of chemotherapy and radiation therapy, with a five year survival rate of more than 90% for early-stage NPC patients, and only about 34-60% for intermediate or advanced NPC patients. Therefore, early diagnosis and treatment of NPC need to be further improved.
Histological classification of NPC
Histopathological diagnosis has long been considered as a ‘gold’ standard for tumor diagnosis. According to the WHO Pathological Classification of Nasopharyngeal Carcinoma (2005), NPC is classified into the following types: type I, keratinizing squamous cell carcinoma, and type II, non-keratinizing carcinoma, the latter of which is further divided into differentiated and undifferentiated subtypes.
Epidemiological data show that 98% of NPC patients in high-incidence areas are type II NPC patients, and only 2% are type I NPC patients. The five year survival status of Type I NPC patients is significantly different from that of Type II NPC patients, whereas there is no significant difference in five year survival status between differentiated NPC and undifferentiated NPC.
NPC exhibits diverse pathomorphologies, which are not significantly associated with its clinical significance.
NPC exhibits diverse pathomorphologies, which are not significantly associated with its clinical significance. Based on this phenomenon, a multicenter cohort study on new pathological classification of NPC led by Professor Jianyong Shao can significantly distinguish those patients, and predict their five year survival status.
The research project included three cohorts: a training group, comprised of patients seen at the Cancer Center of the Sun Yat-sen University between 1995 to 2005; a retrospective validation group, comprised of patients from high NPC incidence areas other than Guangzhou in China, including Guangxi, Hunan, Fujian, Anhui, Hong Kong and Taiwan, as well as Singapore; and a prospective validation group, comprised of patients seen at the Cancer Center of the Sun Yat-sen University between 2007 to 2011.
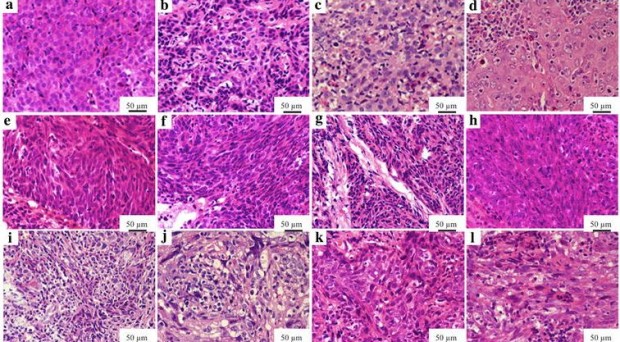
NPC generally exhibits the following pathomorphologies: epithelial carcinoma: small round, oval or cobblestone-like tumor cells, low nucleus to cytoplasm ratio or chromatin-rich cells, ambiguous boundaries between large round cells, centered nucleoli, large and round vesicle-like nuclei, and a nucleolar occupancy in tumor cells of more than 75%; sarcoma-like carcinoma: small irregular cells, large cells with darker chromatin, uniform medium-sized spindle cells with unobvious nucleoli, or tumor cells with darker nuclei and eosinophilic cytoplasm; mixed carcinoma: the characteristics of both epithelial carcinoma and sarcoma-like carcinoma; squamous cell carcinoma: well-differentiated keratinizing squamous cell carcinoma with obvious intercellular bridges and horny pearls, and poorly differentiated or intermediately differentiated squamous cell carcinoma interspersed with a small number of basal-like cells.
This pathological classification offers the following advantages: clear classification boundaries due to distinct cellular characteristics of each type, and ease of being mastered by clinical pathologists.
More importantly, such a classification can predict the five year survival prognosis of NPC patients in the following order: epithelial carcinoma, mixed carcinoma, sarcoma-like carcinoma, and squamous cell carcinoma.
Repeatability and consistency
In order to put the research results into wide use to benefit a vast number of NPC patients, at the beginning of this project in 2008, Professor Shao stated that this new pathological classification method must have good repeatability and be easily mastered by clinical pathologists.
Thus, his research group spent five years visiting more than twenty cities with high NPC incidence including Hong Kong, and Taiwan, and collaborated closely with local pathologists in Singapore.
The research results showed that this new pathological classification had good repeatability, with a 90.2% consistency of reading results among different pathologists.
The research results showed that this new pathological classification had good repeatability, with a 90.2% consistency of reading results among different pathologists.
It was also effective for predicting prognoses of NPC patients among different populations in different areas. This research represents a significant periodical achievement in the studies on molecular classification and individualized diagnosis and treatment technologies for NPC.
We have a responsibility to find potential molecular markers and their mechanisms behind the new pathological classification, which are important for a better understanding of the onset, development and heterogeneity of NPC.
Meanwhile, these molecular markers not only provide molecular biological basis for new pathological classifications, but also lay a foundation for targeted therapy of NPC, and thus open a new chapter in the precise treatment of the disease.
Comments