In 2009 Obama devoted $19 billion to healthcare innovation—innovation that was in its first instance quite rudimentary, the very digitisation of healthcare data. Now as the digitised healthcare data infrastructure grows both in the US and worldwide, what is the next phase of innovation?
The answer, from someone who works with researchers, is clear: a data dialogue between researchers and clinicians. Initiatives like the Global Alliance for Sharing Genomic and Clinical Data led by David Haussler are making strides toward doing this for treatment and research for cancer.
Last week I attended ISMB in Boston, where I saw one quantitative analyst (quant) who had similar ideas about better healthcare treatment through research and more data for research through healthcare. His name was Isaac Kohane. In his talk ’Biomedical Quants of the World Unite! We only have our disease burden to lose’, Kohane puts out a call to all quants. We need to leverage our healthcare system as a high-throughput mechanism for understanding biomedicine.
Healthcare data, especially hospital electronic health records, present an opportunity to study underrepresented populations in biomedicine, populations that are typically overrepresented in healthcare systems.
But in his keynote, Kohane spoke less of what we in research could gain and more of what ’we’ as in the world could gain to healthcare treatment. He appealed to the audience not just as the bioinformaticians who would be doing this work but as consumers of a healthcare system. And that appeal was: Let’s make our data work for us.
Identifying harmful side-effects before the doctors
Take the drug rofecoxib, an anti-inflammatory used to treat arthritis and other chronic pain conditions, that was approved in 1999. Gaining widespread acceptance among physicians, it was eventually prescribed to over 80 million patients worldwide.
However, in September 2004, its manufacturer Merck withdrew the drug finding that it was causing an increased risk of heart attack and stroke. The drug was on the market for five years before this was picked up, as (scarily enough) there is no accepted method for monitoring drug safety in the post launch phase.
Kohane suggests the next logical step is a semi-automated monitoring of healthcare databases, and pointed to research by Brownstein et al, who sought to determine whether automated population health monitoring would have identified rofecoxib as a concern before five years on.
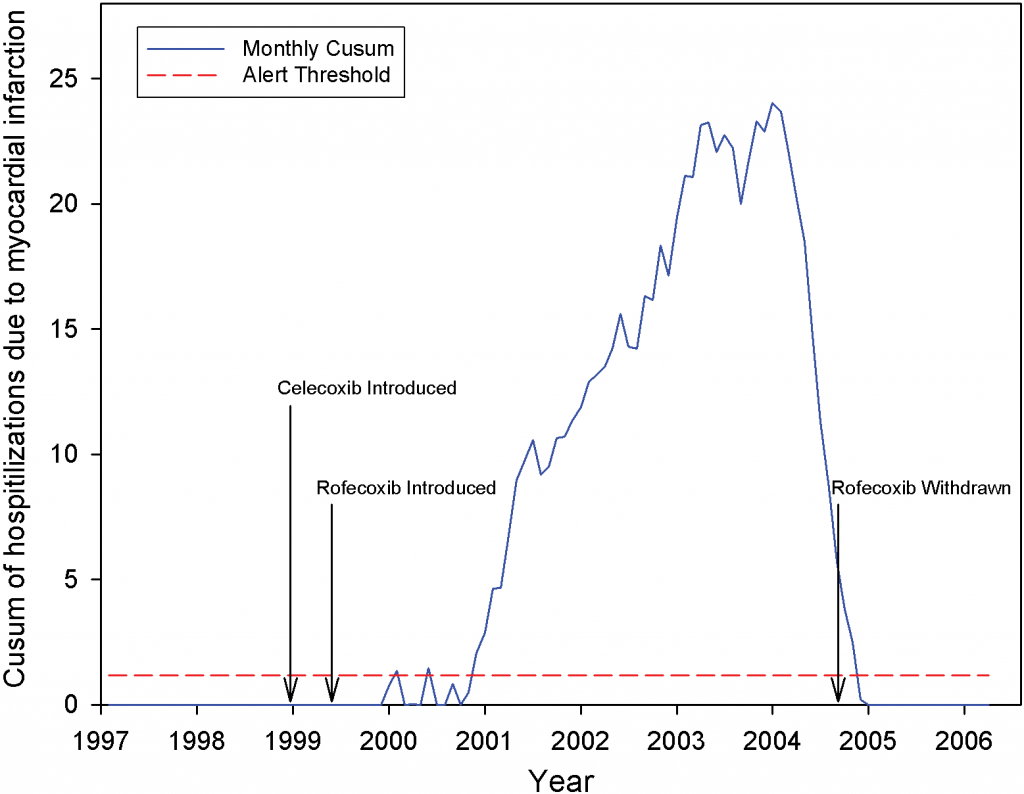
Using data from Massachusetts General as well as other hospitals in the Boston area, they looked for a change in the population rate of heart attacks after the introduction of rofecoxib. As their figure shows, the rate of heart attacks dramatically increase just over a year after rofecoxib hits the market and drops as it is taken off the market.
The questions we are left with are not only how many heart attacks could have been avoided with more systematic post-launch quantitative analysis of drugs, but also how much unnecessary burden is being put on an already overburdened healthcare system purely through an inefficient (at best) feedback mechanism for FDA-approved drugs.
Predicting diagnoses
Another interesting example of the efficiencies and higher quality in healthcare that could be gained from more automated use of quantitative analysis of healthcare data came from the graph below from a study by Reis et al in BMJ.
The study used longitudinal data from historical patient records and Bayesian models to predict patients’ future diagnoses. The aim was to find out whether, through quantitative analysis, the authors could detect a particular diagnosis before a patient was actually diagnosed.
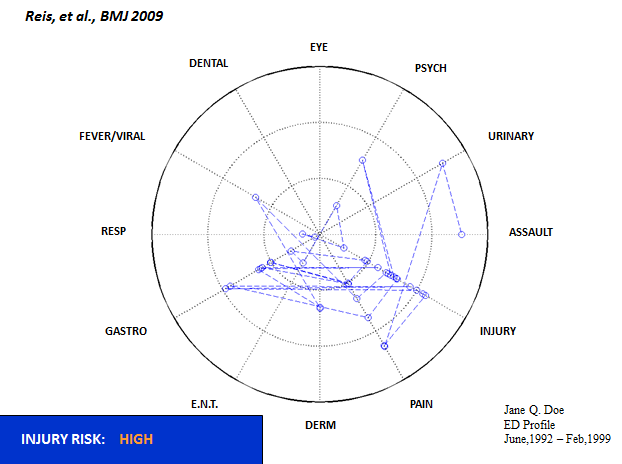
Before reading further, take a look at the graph to the right, which shows one person’s path through the healthcare system from 1992 to 1999, the eventual time of diagnosis. Any guesses as to what the particular diagnosis was for that patient? Only one person in the audience got this right—and he had seen the talk before.
According to Reis et al, “even with unlimited time and resources, assimilating all available information is a difficult task [for a clinician]”. This leads to the missed diagnosis of certain clinical conditions, such as with the above graph, which shows a patient eventually diagnosed with domestic abuse.
In the US domestic abuse can affect up to 16% of couples. Using all the available health system information, Reis et al were able to predict domestic abuse two years before the healthcare system was able to, and up to as much as six years before.
Bringing healthcare into the iPhone era
The benefits to a bioinformatics approach to healthcare are clear. Indeed, as Kohane says, big companies make our data work for them all of the time. Let’s make our data work for us! But how do we make this happen?
Centers like Kohane’s i2b2 center (Informatics for Integrating Biology and the Bedside), which were responsible for the Reis et al. study, are a starting point. Such centers are developing a scalable computational framework to address the bottleneck limiting the translation of genomic findings in model systems relevant to human health.
Kohane’s SMART platform is another. A sort of iTunes for health apps, clinicians and patients. SMART creates a platform to sit on top of electronic health records that allows apps to communicate with these records via an API (something that lets computers talk to each other), analysing and visualising the data they hold.
Apps are being built to help clinicians interpret genomic data but are also designed to help patients understand their own records. For example, take a look at this app to interpret the Reynold’s Risk Score, a commonly used calculation for cardiovascular risk.
However, as an American well familiar with the private insurance system, my first question is who will pay for this on a scalable level? Who will pay to take our healthcare technology from the 80s to the iPhone era?
With the new flow of data from Care.data in the UK, the time seems ideal for the app technology of the iPhone era to take hold. Perhaps, even in the US under private healthcare, the new medical app technology will act as a disruptive force in healthcare, much like open access has for publishing.
I hope so, and as a technologist, this is what I’m placing my bet on. However, Kohane ends his talk by pointing to a much simpler option. “First,” he says, “let’s start publishing papers we want our own family treated with. Quality over quantity.”
One Comment