
Migraine is the most common brain disorder in people aged under 50 years. Migraine attacks occur with external and internal triggers in susceptible individuals. Migraine food triggers such as chocolate, cheese, wine, and citrus fruits are well known, but it is still a mystery how they start a migraine attack. It is also unclear why food triggers do not always cause headaches and why there are certain episodes when migraine patients are more prone to food triggers.
Certain ingredients in these food triggers inhibit a group of enzymes known as sulfotransferases (SULT) which are involved in the detoxification of drugs and chemicals and the metabolism of neurotransmitters and hormones. For example, quercetin and catechin in chocolate, hesperidin in orange and lemon, quinic and caffeic acids in coffee, and epicatechin gallate in tea and red wine inhibit SULT1A1 enzymes.
Migraine attacks are usually treated with nonsteroidal anti-inflammatory drugs (NSAIDs) and the overuse of analgesics transforms migraine into chronic migraine, which is defined as having headaches on more than 15 days per month. Surprisingly, NSAIDs have also been shown to inhibit SULT1A1 enzymes. The mechanism underlying the link between medication overuse and the transformation of migraine is unknown.

We hypothesized that sulfotransferase inhibition was the common mechanism by which food triggers and analgesics synergistically affect migraine susceptibility. Medication overuse by inhibiting these enzymes could make migraine patients more susceptible to triggers, and food triggers even in low amounts could result in chronic headache with exacerbations.
Therefore, we developed a medication overuse headache model by administering mefenamic acid to rats for 4 weeks. We also used hesperidin from citrus fruits. Brain waves and cortical spreading depression (CSD) were recorded using microelectrodes to evaluate cortical excitability and migraine susceptibility. Pain behavior relevant to migraine and anxiety behavior were also assessed. At the end of the experiments, brain samples were collected and SULT1A1 enzyme activity was measured.
We demonstrated for the first time that chronic mefenamic acid significantly reduced CSD thresholds, increased CSD frequency, caused mechanical-thermal hypersensitivity, induced pain anxiety-like behavior and inhibited SULT1A1 enzyme activity. Hesperidin and chronic mefenamic acid exposure together further increased CSD susceptibility and induced pain behavior associated with SULT1A1 inhibition, although single-dose hesperidin alone did not show any significant effect.
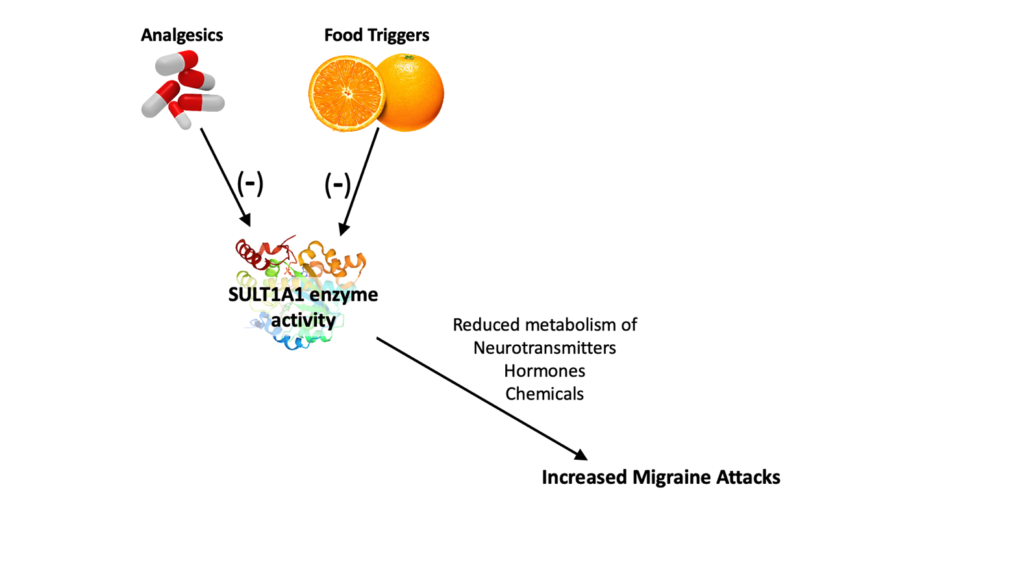
Our research showed inhibition of sulfotransferase enzyme activity as a new mechanism by which analgesic overuse transforms migraine into chronic migraine. We also showed that migraine food triggers via SULT1A1 inhibition may further increase migraine attacks in chronic migraine patients with medication overuse. Chronic analgesic use increases CSD susceptibility and could make the brain more susceptible to the effects of migraine triggers. Under these circumstances, even subthreshold triggers that cannot initiate a migraine attack alone may initiate a migraine attack.
We believe SULT1A1 inhibition is a common mechanism by which medication overuse and migraine triggers affect migraine susceptibility, which may provide a new potential treatment target.
Comments