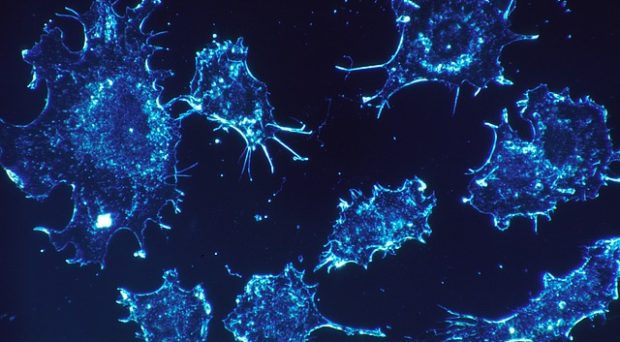
Fundamentally, cancer is a genetic disease driven by genetic mutation. In the fight against cancer, determining the genomic profile for a specific tumor can be extremely powerful for determining the most effective therapy and in discovering novel therapeutic options. Recent advances have highlighted the exciting potential utility from using genomic information to leverage the immune system as a cancer therapeutic.
There is hope that vaccines directed towards these neoantigens will offer therapeutic benefits in cancer patients.
Our immune system is extremely effective at identifying and eliminating foreign pathogens from our bodies – like bacteria and viruses. Fundamentally, this ability stems from its ability to distinguish foreign pathogen protein fragments as ‘non-self.’ These are called antigens. The various offensive and defensive capabilities of our immune system can then be focused to the specific pathogen. To help focus the immune system and produce a robust response, vaccines can be used.
Similarly, we now know that mutations within a tumor can be recognized by the immune-system. Since these are only found in cancer cells, they are termed neoantigens. And just as vaccines are effective against traditional pathogens, like polio and influenza, there is hope that vaccines directed towards these neoantigens will offer therapeutic benefits in cancer patients.
But designing and developing cancer vaccines is much more daunting for many reasons. Cancer sequencing efforts like The Cancer Genome Atlas (TCGA) revealed immense genetic diversity across tumors. For cancer vaccine development, this implies that every patient likely requires a custom-made vaccine specific to their tumor. This limits the utility of this approach since it is extremely technical, difficult to scale, and currently prohibitively expensive for mainstream use. However, the requirement for patient-specific cancer vaccines has not been formally tested across a large collection of tumors.
The Cancer Genome Atlas (TCGA) revealed immense genetic diversity across tumors.
Our study aimed to characterize the genetic diversity of tumors and assess the feasibility of non-individualized cancer vaccines. To do this, we examined genomic profiles from a diverse set of over 63,000 tumors. This revealed that each tumor frequently contains a unique set of mutations. In other words, every tumor is a snowflake.
However, even in the context of this extensive diversity, there were some mutations found across many tumors, albeit rarely together. In fact, we found about 25% of tumors have at least one mutation from a set of only 10 (selected to maximize the number of tumors containing at least one of these mutations). This means that if a cancer vaccine could be developed against these 10 mutations (a poly-neo-epitope vaccine), it may be an option for up to 25% of cancer patients – an intriguing finding that could make cancer vaccines a more feasible therapeutic option.
In other words, every tumor is a snowflake.
But we know that not all mutations are able to be recognized by the immune system. We thus applied state-of-the-art algorithms that predict which mutations can be recognized by the immune system. In a best-case-scenario analysis, this revealed that a non-individualized cancer vaccine approach could be feasible, but would be limited to less than 1% of the cancer patient population.
Our study provides invaluable data to help guide cancer vaccine development efforts. There are important limitations to our study but they provide strong evidence that cancer vaccines and other targeted immunotherapies will likely need to rely on individualized approaches for the clear majority of cancer patients.
Comments