

My colleagues and I became interested in cancers caused by particular herbal remedies through an ongoing collaboration with Dr. See-Tong Pang in Taiwan. In grim irony, while these herbal remedies were often taken for weight loss, they contained a chemical that is intensely mutagenic and an acute kidney toxin.
The offending plants are a group of species in the genus Aristolochia, which often have beautiful flowers called ‘Dutchman’s pipes.’ These plants have been, and likely still are, used in traditional medicines in many areas of the world, including East and South Asia and South America.
Mutation signatures of aristolochic acid and cancer
The toxic and mutagenic chemicals in these plants are aristolochic acids (AA). Chemical derivatives of AA physically link to bases in our DNA, thereby damaging it and causing mutations. AA leaves a distinctive mutation signature in the form of a strong preference for A > T (adenine to thymine) mutations in particular genomic contexts. This signature has not been linked to any other mutagen.
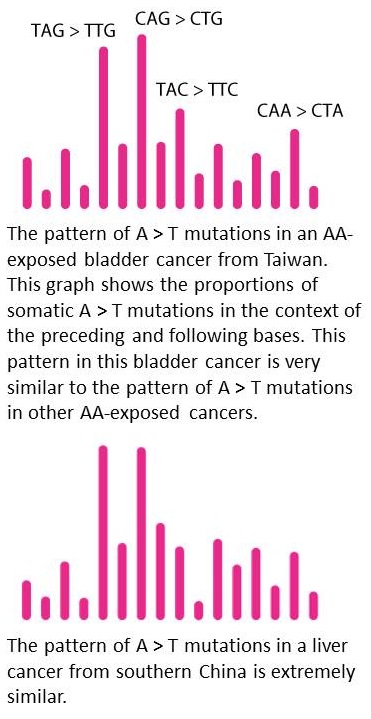
AA was known to cause kidney failure and upper-tract urothelial cancers in Taiwan and in hot-spot areas of the Balkans, where AA-containing seeds were accidentally harvested along with wheat. However, as we were studying mutations in liver cancers from Southern China for another project, we noticed the same pattern of A > T mutations.
Following up on this, this week’s article shows AA signatures in bladder cancers from Taiwan, China, and Singapore. Meanwhile, other research groups have found AA signatures in yet another urological cancer, renal cell carcinoma, in areas of the Balkans not previously thought to be hotspots for AA exposure.
Our understanding of AA mutagenesis in cancer has advanced rapidly in the last few years. While a few years ago we knew that AA caused upper-tract urothelial cancer, we now also know of, or strongly suspect, AA involvement in cancers of the bladder, kidney, bile duct, and liver.
In terms of geographical regions at risk, we now have molecular evidence of AA involvement in cancer in China and Singapore, while previously this was only suspected based on likely use of AA-containing herbs. We also know now that AA exposure is more widespread in the Balkans than just the hot-spots for AA kidney failure. Although I have seen no molecular evidence of AA exposure in cancers from South Asia or South America, AA-containing herbal remedies probably still used in both areas.
From mutation signatures to cancer prevention
The ever-mounting evidence of the importance of AA in multiple types of cancer and regions of the world should lead to more extensive efforts in primary prevention – avoidance of ingesting AA-containing plants. This could occur through further regulation and education.
Arguably, since AA is not addictive, this would be easier than prevention of tobacco smoking. It is worth commenting that under the Dietary Supplement Health and Education Act of 1994, botanical products are basically unregulated by the US Food and Drug Administration (FDA), provided no health claims are made. The FDA has, however, urged manufacturers and distributors to ensure that botanical products are free of AA, and it has advised consumers to avoid products containing AA.
Beyond primary prevention, patients with known or suspected AA exposure might benefit from intensified screening for associated cancers; patients with kidney failure due to AA ingestion might fall in this category.
Wider implications for cancer epidemiology
I would like to generalize the approach of using mutation signatures to infer carcinogenic exposures – an approach that has been successful with AA – to other mutagenic carcinogens. In fact, some 30 mutation signatures have been recognized in compendia of somatic mutations from over 10,000 tumors. Of these signatures, only 6 are linked to known exogenous factors, while 14 have unknown causes. (The remainder are due to endogenous mutagenic processes, such as DNA mismatch repair deficiency.)
Conversely, the signatures of numerous known mutagenic carcinogens are unknown. Furthermore, the next 10 years will see somatic mutation compendia from hundreds of thousands of tumors from many parts of the globe, and some of these will bear the signatures of mutagens present in specific geographic regions or due to specific occupational exposures. Thus, there is a molecular epidemiological opportunity to link mutagens to their signatures, determine their impact on the burden of cancer, and adopt preventive measures.
A major prerequisite for this vision of wide use of mutation signatures in molecular cancer epidemiology will be development of robust cell-culture-based systems for inexpensively assessing mutation signatures. Such systems would be important not only for molecular epidemiology, but also for safety testing of compounds. Another prerequisite for wide use of mutation signatures in molecular epidemiology will be improved tracking of clinical and demographic information, as well as possible carcinogen exposures, associated with sequenced tumor samples.
Prevention is a powerful weapon in the fight against cancer, with the effectiveness of tobacco suppression in reducing lung cancer as a prime example. Improved information about the actual carcinogenic burden of other known or suspected mutagens presents an opportunity to target the most important mutagens for further prevention efforts.
Comments