Guest blog post by Dr Carlo Galli, author of a timely Commentary published in Journal of Negative Results in BioMedicine, which discusses the debate surrounding seratonin in the treatment of bone loss in periodontitis. He argues that although contradictory, recent findings may lead the way to novel treatment opportunities for periodontitis and similar bone loss.
One of the crucial aspects of approaching a disease is understanding what is causing it, and this is often overlooked with periodontitis. Periodontal therapy still mostly relies on mechanical removal of plaque and calculus, based on the assumption that they are the main factors responsible for the progress of this disease. Why periodontitis arises in certain patients but does not in others however is mostly unknown – and more importantly – ignored. Therefore how to modulate the host response to hamper periodontal damage is still out of the clinician’s grasp. The transfer of advanced concepts from bone biology to periodontics, much like the influence of oxidative stress on alveolar bone loss, is a somewhat recent achievement and consideration of this issue is very limited.
Understandably, this holds even truer for controversial topics, such as the effect of serotonin on bone. Yet the recent publication of research on the effects of selective serotonin reuptake inhibitors (SSRIs) calls for more exploration of this issue: research undertaken by Banco del Almeida et al. and Carvalho et al. examines the effects of SSRIs on animal models of periodontitis, and their intriguing findings will be discussed below.

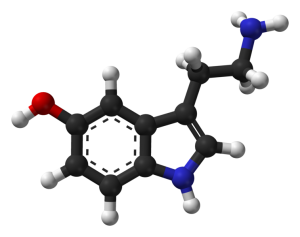
Serotonin, or 5-hydroxytryptamine (5-HT), is a neurotransmitter that is known to regulate mood and behavior by acting on the central nervous system. Interestingly, it can also be synthesized by completely different sets of cells, such as heterochromaffin cells in the gut, endothelial cells in the lung, or platelets, thus forming self-standing signaling systems. Whether serotonin goes beyond the central nervous system and reaches bone, is the object of a fierce debate. Wnt signaling is one of the most significant signaling pathways for bone accrual and maintenance, and this debate is jeopardizing the whole idea of how it operates in bone.
What is currently maintained is that canonical Wnt signaling is triggered by Wnt factors binding to a membrane receptor dimer including some Lrp isoforms, like Lrp5, on bone cells. Some data however show that Lrp5-/- mice have increased serotonin blood levels and the low-bone mass phenotype of these mice can be simply rescued by removing serotonin precursor tryptophan from the diet. Consistent with this data, gut specific activation of Lrp5 has been observed to increase bone mass in rodents. The somewhat revolutionary hypothesis put forth mainly by Dr. Karsenty’s group at Columbia University is therefore that canonical Wnt signaling does not directly act on bone cells but rather on serotonin-producing cells, which then act on bone cells. Although there is equally solid evidence that fails to confirm these observations or plainly contradicts them, several works show that SSRIs are significantly associated with increased risk of bone fracture. They also demonstrate that polymorphism of the 5-HTT transporter gene affects bone phenotype, and last but not least, is associated with aggressive periodontitis.
This is more than enough reason to look with great interest at SSRIs studies in periodontitis, and the two aforementioned studies, perhaps unsurprisingly, yield conflicting results. Branco de Almeida et al. showed that the SSRI fluoxetine improved the outcome of ligature-induced periodontitis in rats, while Carvalho et al. reported that the SSRI venlafaxine increased bone loss in a similar in vivo model. The fact that both drugs actually affected periodontitis is curious, but why they had opposing effects is baffling. These studies provide few clues as to why this is the case, because they were not designed to test the hypothesis that the control of serotonin reuptake could affect alveolar bone loss. They simply test the hypothesis that antidepressant drugs could be effectively used in periodontal therapy.
Fluoxetinehas indeed been proven to inhibit several metalloproteinase enzymes, which are known to participate in periodontal destruction, and control osteoclast viability. Interestingly, fluoxetine has also been observed to have differential effects on cortical or trabecular bone compartments, all of which should be considered when trying to answer this question. Furthermore, Yadav et al., showed that serotonin in the central nervous system has the opposite effect on bone than peripheral serotonin; in addition to this, inhibition of its synthesis actually negatively affects bone mass. It is also possible that different drugs may have a bigger impact on one serotonin pool rather than the other.
So why is it important to try and solve this conundrum instead of just focusing on other simpler treatment approaches? Periodontitis has a microbial trigger, but alveolar and periodontal destruction is primarily driven by the host response. It is becoming more and more apparent that treatment of periodontitis cannot be limited to debriding periodontal lesions, which is often an incomplete procedure and is dependent on clinical expertise and patients’ compliance. Therefore, if serotonin was confirmed to be capable of modulating pathways that control bone formation, it could be a key factor in blocking or reversing periodontal bone loss in the use of systemic or topical drug therapy. Also worthy of note is LP533401, a novel compound which has recently been generated. In vivo studies have shown that it can indeed increase bone mass, although no data is available about alveolar bone yet.
It may be an uncertain time for the serotonin debate, but it may be a promising time for new treatment opportunities.
Dr Carlo Galli is a Research Associate at the University of Parma, and carries out research on the interactions between implantable biomaterials for bone regeneration and cells.
Journal of Negative Results in BioMedicine is keen to publish insightful discussion of unexpected findings in order to provide the scientific community with more accurate and reliable information. Submit your unexpected or controversial results at https://www.jnrbm.com/manuscript. Follow us on Twitter: @JNRBM.
Comments