Immunotherapy has changed the landscape of cancer treatment, providing benefit across a range of diseases once considered untreatable and extending the lives of these patients.
These effects have been observed in a growing number of cancer types, including melanoma, non-small cell lung cancer, and bladder cancer, leading to multiple FDA approvals. However, the harsh reality is that most patients will not respond to these new therapies, with response rates ranging from 15-40%.
Most patients will not respond to these new therapies, with response rates ranging from 15-40%
Coupled with the high cost and risk of serious immune-related side effects, there is an urgent need to identify reliable, quantitative biomarkers, capable of identifying those most likely to benefit.
One such biomarker which has been associated with response to immunotherapy in multiple disease types is tumor mutational burden (TMB). TMB measures the number of mutations within a tumor genome, and tumors which harbor more mutations have been shown to have a greater likelihood of response to immunotherapy.
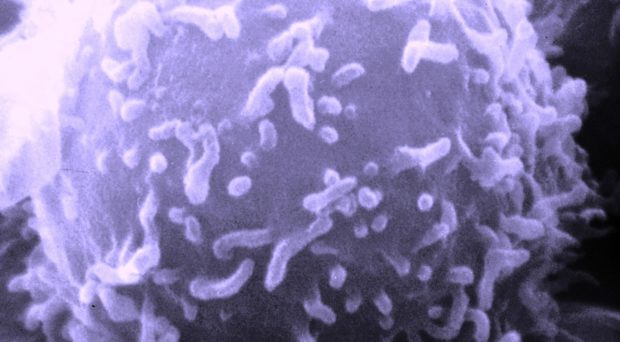
Researchers have hypothesized that the increased mutation rate leads to an increased number of mutated proteins, or neo-antigens, on the surface of tumor cells capable of eliciting an immune response. This pre-existing immune potential is a major factor that will determine whether patients derive benefit from immunotherapy.
Methods of measurement
One of the first established methods evaluated the expression of the PD-L1 protein on the surface of tumor cells through immunohistochemistry (IHC); however, this method has been difficult to universally adopt, and the qualitative nature makes interpretation of the results tough to refine.
Another method involves the detection of the specific neo-antigens in the tumor genome; however, this relies on whole exome and transcriptome sequencing, which can be very costly and time-consuming. The measurement of TMB offers an alternative to neo-antigen detection, using the mutation rate itself as a proxy for the neo-antigenic burden.
TMB had previously been shown to predict response to immunotherapy when measured using whole exome sequencing.
Comprehensive genomic profiling
TMB had previously been shown to predict response to immunotherapy when measured using whole exome sequencing, sequencing of all the coding regions of the genome (~20,000 genes). In this study, we tested whether TMB could be accurately measured by a targeted comprehensive genomic profiling (CGP) panel of 315 genes.
We found that measurement by CGP was highly correlated with measurement by whole exome sequencing. We further calculated the variation in measurement when sequencing less than 315 genes. As expected, the accuracy of measuring TMB declined as fewer genes were sequenced.
To better understand the applicability of TMB as a biomarker across a wide variety of cancer types, we measured TMB across more than 100,000 patients with diverse, primarily metastatic cancers from our clinical cohort.
These data help to characterize the distribution of TMB across many cancer types and identify those which harbor a significant proportion of patients with elevated TMB, which may make them good candidates for clinical trials testing immunotherapies.
Overall, we found 22 cancer types across 8 tissues with >10% of patients who had high TMB. In addition, we found that in nearly every cancer type evaluated, there existed some patients with high TMB.
We also identified novel, recurrent mutations in the promoter of the PMS2 gene in melanoma patients with increased TMB. These mutations are quite common in melanoma, occurring in approximately 10% of melanoma patients in our cohort.
The PMS2 protein is involved in the mismatch repair pathway, repairing damage to DNA. Mutations within the coding region that disrupt the normal protein function are known to cause increased mutation rate.
Our data across many cancer types helps to characterize the distribution of TMB in many previously uncharacterized cancer types.
Similarly, the mutations we identified within the promoter region may lead to an increased mutation rate by disrupting the normal expression of the protein, although establishing this causative relationship will require additional studies.
Overall, TMB has been shown to be a predictive biomarker for distinguishing which patients may respond to immunotherapy. Our data across many cancer types helps to characterize the distribution of TMB in many previously uncharacterized cancer types and may help to inform clinical trials for immunotherapies. Finally, we show that this biomarker can be accurately measured with a widely available, comprehensive genomic profiling assay, demonstrating that this is a cost-effective and clinically viable method for measuring TMB.
Comments