
Please could you tell us a bit about the European Association for Predictive, Preventive and Personalised Medicine and the working group who present this position statement?

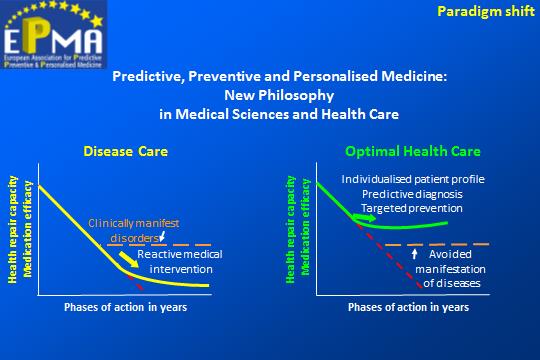
EPMA (www.epmanet.eu) with 47 country members (Europe and world-wide), was created in 2008 in order to promote a paradigm shift away from “unPPPM” which is characterised by delayed intervention, untargeted medication, overdosed patients, and ineffective treatments to predictive, preventive and personalised medicine (PPPM) in medical sciences and healthcare systems on the European and global scale.
Due to its multifaceted advantages (such as clear concepts and advantages to the patients, multi-professional approach, great technological innovation and advanced economy of healthcare), PPPM is considered the medicine of the future.
The dedicated working group who created the EPMA Position Paper 2016 consists of experts actively involved in world leading organisations, scientific groups and medical centres with a whole spectrum of expertise ranging from traditional medicine to innovative technologies, medical ethics, law and healthcare economy.
Please could you summarise the key findings that you wish to convey in your position statement?
The ethical imperative of medicine is to identify the right patient treating them with the right medication and the right dose at the right time
Several approaches have been suggested in ancient and modern medicine to conduct medical services in an optimal way. Currently there are too many different names of medicine, frequently confusing patients and even professionals. What is the difference between ‘Person-centred’, ‘Individualised’, ‘Stratified’, and ‘Precision’ medicine, amongst others? How big is the potential beyond corresponding approach to satisfy the needs of the individual, the patient, professional groups involved and society at large?
The dedicated EPMA working group provides a deep analysis of the issue followed by the expert recommendations considering the multifaceted aspects of both “disease care” and “health care” practices. Conclusion and recommendations are summarised in Table 1 presented in the paper. The most optimal system effectively advancing healthcare systems on a global scale is imaged below.
Why is this an important topic for the future of medical healthcare?
The ethical imperative of medicine is to identify the right patient treating them with the right medication and the right dose at the right time. However, good but empty slogans are not helpful – they should be achievable and this requires a feasible approach.
A citizen with an actual or potential disease wants a medicine in which they are at the centre, a medicine which is tailored to their individual patient profile, a medicine which is able to predict and prevent possible diseases. They are not interested in the actual classification term of this kind of medicine; however they are interested in the reasoning behind the classification of the medicine, in order to appreciate its potential ability to restore health. And this is the real advantage of speaking in terms of Predictive, Preventive and Personalized Medicine: the patient understands what is going on!
PPPM lends itself to an over-arching umbrella under which the main ethical issues of contemporary biomedicine could be positively tackled. Certainly a predictive and preventive approach could imply several ethical problems. For example: over-diagnosis and overtreatment; detection of incidental findings; psychological burden and severe existential choices connected with the potential for a disease to be passed onto our offspring.
Contextually, PPPM plays a crucial role as the optimal medical partner of serious ethical counselling offered to actual or potential patients, in order to empower them to make an informed choice about the diagnostic, surveillance or therapeutic path to take; especially when these paths intersect ethical or existential problematic situations that they have to solve.
Comments