Will we ever know what causes this blood vessel destroying disease? What lessons can we learn from other diseases and how can a study such as ours help in that process?
Why don’t we look at another disease as an example…
Imagine if you knew everything there was to know currently about coeliac disease except what causes it – wheat gluten. How would you go about identifying that causative factor?
You would know it’s presenting symptoms and that those symptoms were due to chronic inflammation in the small intestine resulting in malabsorption suggesting an ingested causative factor
You would know that while gastrointestinal symptoms are the most common presentation occasionally skin and cerebellar symptoms predominate and rarely gastro-intestinal symptoms may be absent. These observations may confound you.
You would know there are genes encoding certain antigen receptors – HLA DQ2 and HLA DQ8 -that present an autoantigen called tissue transglutaminase to the immune system and that the detection of serum autoantibodies to tissue transglutaminase have both high diagnostic sensitivty and specificity.
How does this fit with GPA?
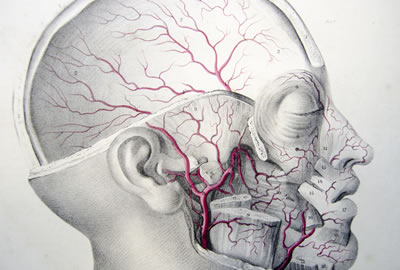
We know that GPA is a chronic potentially life-threatening multi-organ disease that results from destruction of small arteries and arterioles.
Currently we are in a similar position with respect to GPA only it is a much less common disease. Arguably a more informative name is perhaps anti- neutrophil proteinase 3 associated small vessel vasculitis.
We know that GPA is a chronic potentially life-threatening multi-organ disease that results from destruction of small arteries and arterioles with a predilection for those of the sinuses, upper airways, lung parenchyma, kidney and skin.
We know that certain genes encoding antigen receptors – HLA-DPB1 and HLA –DPA1 – are more common in patients with GPA than in the general population.
We know that the serine protease, human neutrophil proteinase 3, is a very important autoantigen and that serum anti -PR3 autoantibodies have both high diagnostic sensitivity and specificity.
But we don’t know the cause.
It was Willem Dicke, a Dutch paediatrician, who made the seminal observation in World War II that removal of bread from the diet of his paediatric coeliac patients lead to a marked improvement in their symptoms and that its re-introduction worsened them. It was much latter that certain circulating serum antibodies were characterised as disease markers and as a result the broader clinical spectrum of coeliac disease was recognised.
Different threads of information point to an environmental trigger for GPA however the relative rarity of the disease hinders identification.
Different threads of information point to an environmental trigger for GPA however the relative rarity of the disease hinders identification. It is unlikely that observational studies such as Dicke’s will lead to its discovery. Case control and other epidemiological studies such as ours while not definitive help narrow down the potential source of candidate antigens. Identification of the trigger will likely come from testing in suitable animal models.
Despite the study’s limitations, it has essentially replicated the result of a similar study from the Northern hemisphere.
Both studies point to a restricted group of inhaled antigens as a potenital source for the trigger of GPA. It is hoped that such findings will help triangulate future threads of information narrowing the focus in the hunt for the cause.
Comments