Neglected Tropical Diseases (NTDs) are a group of 17 infectious diseases caused by pathogenic viruses, protozoa, helminths and bacteria. As a group, the socio-economic impact of NTDs on countries where they are endemic is comparable to malaria, AIDS or tuberculosis but, as you might guess from the term ‘neglected’, research into them doesn’t receive as much funding or attention.
We tend to consider NTDs as a problem for tropical areas of Asia, Africa and the Americas, but just because they are traditionally a burden to these regions, doesn’t mean that they can’t be a real issue for people from outside the tropics.
With climate change we are seeing (and will continue to see) the migration of parasite vectors from tropical regions to more temperate locales. In addition to this, population displacement due to war or environmental causes (e.g. drought) exposes people who would not otherwise have been at risk to NTDs.
Finally, as people are now much more mobile than in past generations, and international travel – either for leisure or work – is on the rise, more and more people are experiencing tropical infections first hand. This was the case for Marcus Brent Smith from the UK.
A case in point…
Marcus travelled to the Manu region of South East Peru to work as a videographer and photographer for a conservation NGO. He spent ten months there and during this time he developed leishmaniasis.
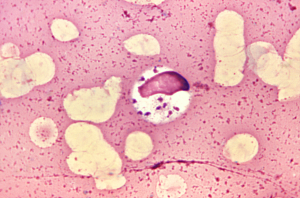
Leishmaniasis, one of the Neglected Tropical Diseases, is caused by protozoan parasites of the Leishmania genus and is transmitted from mammal to mammal via infected sand flies during feeding.
The most deadly form of the disease is visceral leishmaniasis – or Kala-azar – and if left untreated will lead to death. The World Health Organisation report that approximately 1.3 million people contract leishmaniasis each year and 20 to 30, 000 people die as a result.
Before he travelled to Peru, Marcus consulted a travel nurse, but leishmaniasis was not flagged as a risk and he found that not many people knew about the disease in the UK. He was, however, alerted to the potential risks from friends who had contracted the disease whilst travelling, and from colleagues working in the region.
“I couldn’t tell you when the actual bite happened,” says Marcus, “but I first noticed a small cut with a small scab on my upper left tricep in August. It was only a few millimetres across and it looked like a small, round scratch.
“When it had healed and the scab lifted off, the skin underneath was raw and bleeding instead of pink and healthy. Once this happened for a second time my suspicions were aroused. By the end of September the lesion had not healed and had grown to perhaps 5mm across so I knew that it was Leishmaniasis.”
 Treatment was available in Peru for leishmaniasis, but to obtain it he would have had to make a three hour round trip to the local medical centre (by boat and on foot) each day. On top of this, a side effect of the treatment is that it made you weak, and so would make walking difficult.
Treatment was available in Peru for leishmaniasis, but to obtain it he would have had to make a three hour round trip to the local medical centre (by boat and on foot) each day. On top of this, a side effect of the treatment is that it made you weak, and so would make walking difficult.
This highlights the difficulty healthcare workers have in ensuring that locals with leishmaniasis can actually get the treatment they need. Marcus obtained treatment for leishmaniasis back in the UK – initially consulting the Hospital for Tropical Diseases in London who confirmed that it was leishmaniasis, and then getting treatment from a local hospital in Oxford.
Six months later, all that is left to remind him of the disease is scar the size of a fifty pence piece.
Marcus has read a great about leishmaniasis since his infection and his advice to people visiting an area where leishmaniasis is a risk is: “the rules are the same as for malaria: avoid getting bitten. So cover up with trousers and long sleeves, avoid exposure at dawn and dusk and wear some insect repellent.”
With global warming, population displacement and increased travel and trade, NTDs are becoming a real risk to people who would not normally otherwise come into direct contact with them. Meanwhile, challenges in healthcare delivery continue to make them a deadly risk to local populations. There’s clearly a need to increase funding and research into these diseases, ideally enough that we can drop the word ‘neglected’ from their collective name.
Comments