Multiple disea ses are covered by the umbrella of poorly understood etiology coupled to an exaggerated or misguided inflammatory response. At first sight, it might seem odd that conditions as different as rheumatoid arthritis and Crohn’s disease are grouped together, but a closer look reveals that although the affected tissue is different, there are actually many common pathogenic processes. A good example is the involvement of the pro-inflammatory cytokine TNF-alpha.
ses are covered by the umbrella of poorly understood etiology coupled to an exaggerated or misguided inflammatory response. At first sight, it might seem odd that conditions as different as rheumatoid arthritis and Crohn’s disease are grouped together, but a closer look reveals that although the affected tissue is different, there are actually many common pathogenic processes. A good example is the involvement of the pro-inflammatory cytokine TNF-alpha.
Monoclonal antibodies that target TNF-alpha, such as infliximab, are used in the treatment of both diseases. However, the efficacy of the treatment can vary, and some patients can undergo long periods of therapy with no observable benefit. What if it were possible to predict beforehand which patients will respond to therapy and which will not?
A recent study in Genome Medicine from the team led by Laszlo Nagy proposes a non-invasive approach to monitor 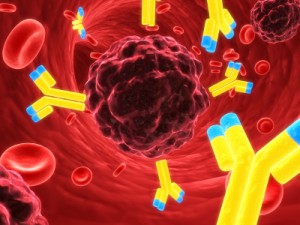 the response to anti-TNF-alpha therapeutics in rheumatoid arthritis and Crohn’s disease patients. Analysis of gene expression profiles of peripheral blood mononuclear cells revealed gene panels that can determine, before therapy starts, which patients will respond to infliximab in both diseases. Interestingly, despite the similarity in the pathogenic processes underlying rheumatoid arthritis and Crohn’s disease, these gene panels turned out to be mostly non-overlapping.
the response to anti-TNF-alpha therapeutics in rheumatoid arthritis and Crohn’s disease patients. Analysis of gene expression profiles of peripheral blood mononuclear cells revealed gene panels that can determine, before therapy starts, which patients will respond to infliximab in both diseases. Interestingly, despite the similarity in the pathogenic processes underlying rheumatoid arthritis and Crohn’s disease, these gene panels turned out to be mostly non-overlapping.
This not only has important clinical implications, but also economic, as anti-TNF-alpha monoclonal antibodies, like all biologic agents, have a high cost. Distinguishing patients that will benefit from anti-TNF-alpha therapy and those who might require a more personalized approach will allow more efficient clinical management of these chronic diseases.
Comments